Drive financial performance with AI-native software and services
Medical Billing and Practice Management
Maximize your collections and operational efficiency with athenaOne’s AI-native medical billing and practice management software and services. Smarter workflows mean fewer denials, less manual work, and faster payments.
Collect more, faster, with AI
Accelerate your reimbursements with AI-native automation that supports cleaner claims, faster posting, and fewer denials, helping you collect more with less effort.
Claim scrubbing and AI follow-up
Reduce denials and speed-up collections with our automated rules engine and AI-native Claim Alarms that identify the optimal time to follow up.
Automatic payment posting
Collect payments faster and lighten staff workload with automated payment matching and posting, verified for accuracy by our expert team.
Automated denial advice
Take the guesswork out of coding-related denials with easy-to-understand, AI-generated coding advice that helps resolve denials quickly.
AI-driven front-office efficiency
Improve your team’s productivity with AI-driven workflows that help reduce manual work, boost accuracy, and drive smoother operations.
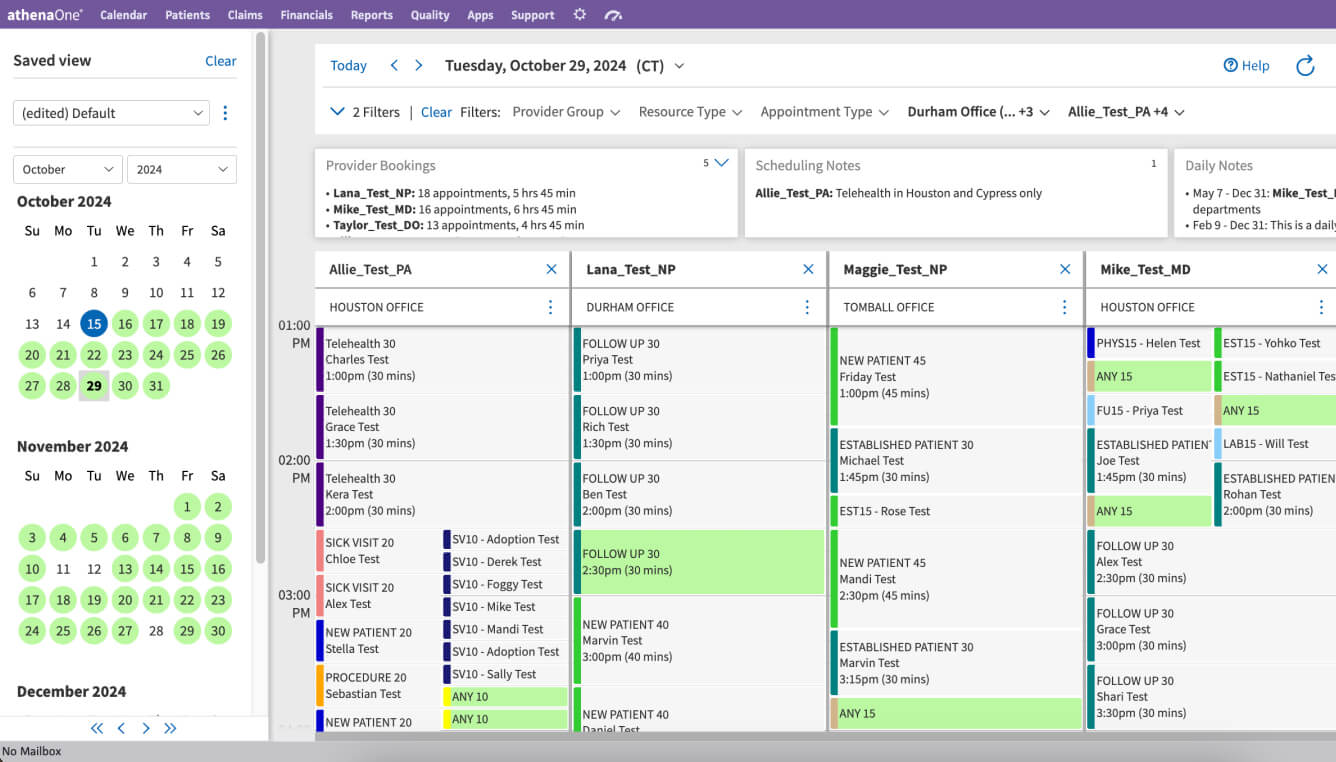
Streamline scheduling
Let AI-driven Waitlist Scheduling automatically refill cancelled appointments by scrubbing current patient waitlists and contacting them to fill the open spot.
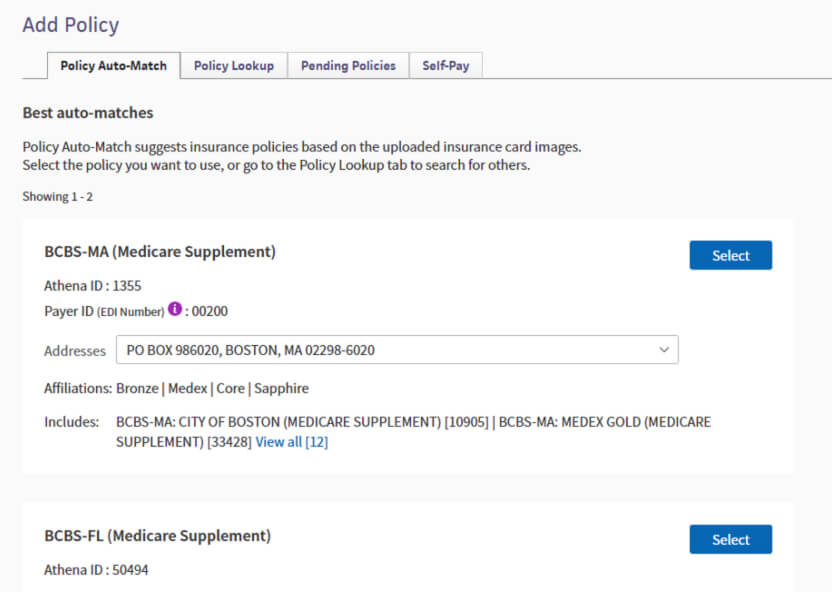
Automate insurance verification
Save time and avoid denials with AI support that instantly extracts and verifies insurance information from patient card images.

Simplify patient payment
Increase patient collections through flexible tools that manage copays, prepays, and payment plans across digital and traditional channels

AI copay prediction
Increase collections while building patient trust with AI support that will predict more accurate patient copays at the time of service.
Intelligence that elevates performance
Help your organization thrive financially with improved performance visibility, comprehensive data reporting, and expert insights from ongoing research.
Network insights
Enhance your performance with automatically integrated learnings from our proactive, AI-driven payer research and continuously updating rules engine.
Easy-to-use reporting
Make better-informed decisions with near real-time visibility into your financial performance and reports that help you monitor your business’s most important metrics.
Executive summary dashboards
Understand key financial performance indicators at-a-glance and identify actionable insights that help drive continuous improvement.

Our 4th year at #1 Best in KLAS
We’re proud to be ranked #1 Best in KLAS 2026 for Practice Management, 11-75 Physicians, Independent – for the 4th straight year.
athenaOne
Expanded RCM Capabilities
Explore these additional services and AI-powered tools for reclaiming staff time and accelerating your collections.
One solution. One partner. One goal - your success.
athenaOne
*This customer is part of our Client Advocacy Program and was not compensated for this content.