Embracing value-based care: Insights for physicians and staff

The Centers for Medicare and Medicaid Services (CMS) have established the requirement that by 2030, all Medicare beneficiaries must be in an “accountable care” or value-based Quality Payment Program (QPP). Every year as 2030 approaches, medical practices must ensure that more Medicare participants are in care relationships with accountability for quality and total cost of care until 100 percent value-based care (VBC) coverage is reached in 2030.1
In addition to CMS requirements for QPP participation, many large healthcare payers are also including value-based payment models as part of their provider contracts. It’s no secret that the transition to value-based care is rapidly changing the healthcare industry.
As a healthcare professional, understanding this evolving landscape of value-based care is crucial not only for the strategic direction of the industry, but also for supporting physicians and practices in navigating this transition. A recent survey sponsored by athenahealth2 highlights both the opportunities and challenges associated with VBC, shedding light on the sentiment of physicians across the United States.
In this post, we’ll unpack some of these insights from physicians using value-based care payment models and discuss what they mean for our healthcare ecosystem as more practices move to implement VBC contracts into existing fee-for-service models.
Current Landscape of Healthcare Payment Models
According to the 2023-2024 Physician Sentiment Survey, the predominant payment model in the US remains fee-for-service (FFS), with 41.6% of respondents relying exclusively on it. Data surrounding the usage of healthcare payment models showed that 10.4% of respondents operate exclusively under a value based care model, and another 38.8% use a hybrid approach of FFS and at least one quality payment program (QPP) such as MIPS for Medicare Part B.
This data suggests that while there is an openness to value based healthcare, many practices are hesitant to fully commit, likely due to the financial risks inherent in these models. Large academic medical centers, for example, may face unique pressures that complicate their transition to VBC, as existing workflows and financial relationships can make change more difficult. However, these same larger systems may benefit the most from the stable revenue that value-based care contracts offer and have the resources to implement technological shifts that make using, reporting, and succeeding under VBC programs more efficient and effective.
The potential of Value-Based Care to manage healthcare costs
According to the 2023-24 survey results, physicians recognize the potential of VBC to significantly impact healthcare costs, ranking it as the second-most-cited factor for managing these expenses (selected by 15.1% of physicians). This finding provides further evidence that physicians see the economic benefits of VBC and aligns with broader discussions within the industry about healthcare cost management strategies and the rationale behind the 2030 VBC mandate.
Price transparency emerged as a top concern among physicians in general. There were no statistically significant differences between VBC and FFS physicians, indicating a widespread desire to align healthcare cost and quality, regardless of their payment model. Sentiment toward price transparency may be something to track in future years as new regulations around the disclosure of payer-provider negotiated rates go into effect.
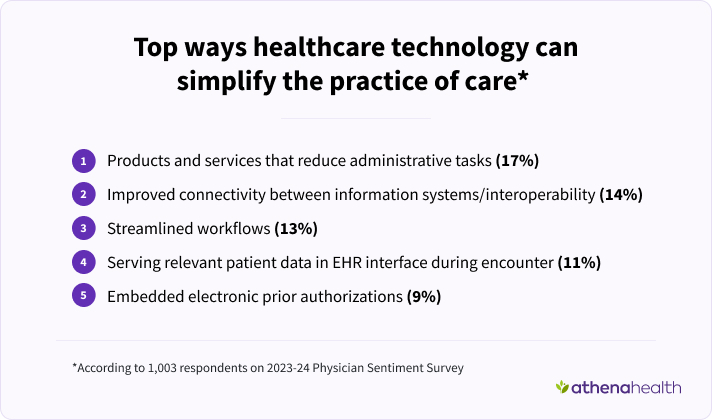
The importance of interoperability and eased administrative burden
One key finding is the contrast in perceptions of information system connectivity between VBC and FFS practitioners. FFS physicians are 32% less likely to believe that improved interoperability between systems could substantially influence cost management (11.5% of exclusively FFS physicians compared to 16.0% of physicians using any form of VBC). This suggests that those engaged in VBC are already experiencing the benefits of data integration and streamlined workflows essential for delivering high-quality care and meeting value-based care program requirements, which include cost containment.
As athenahealth research has shown, interoperability reduces complexity around data silos, streamlines workflows, and shifts the focus to delivering high-quality care – all of which are critical to successful VBC.
Moreover, exclusively VBC practitioners report that their Electronic Health Records (EHR) systems are more effective in reducing administrative burdens. In fact, they are 1.9 times as likely to agree or strongly agree that EHRs help lessen the time spent on administrative tasks compared to their FFS counterparts.
This difference highlights the potential for VBC to not only enhance patient care but also improve operational efficiencies. It also aligns with previous research demonstrating that the fragmentation of FFS payment models (e.g., multiple transactions, potential physician-insurance disputes) creates both a higher cost and administrative burden.
Technological Innovation and AI: A Shifting Paradigm
Another noteworthy insight from the 2023-2024 Physician Sentiment Survey is the willingness of exclusively VBC physicians vs fee-for-service only practices to adopt emerging technologies, including artificial intelligence (AI). Exclusively VBC physicians are 2.1 times as likely to view AI as a means of alleviating physician burden. These findings echo recent work from the American Medical Association (AMA) which suggests that AI may streamline operations, increase cost efficiency, and improve patient outcomes among VBC practices.
As we continue to explore technological advancements including AI, it’s essential for healthcare organizations to support physicians in harnessing these tools effectively to drive better patient outcomes.
Navigating Financial Risk with Value-Based Care Contracts
The 2023-24 survey also revealed that a sizable portion of VBC physicians—31.8%—feel they bear substantial financial risk3 for their patient populations, compared to 17.4% of physicians overall4. This disparity highlights the trade-offs inherent in VBC models, where financial responsibility is tied to performance metrics for cost and quality, and why a shift to value-based care models requires a shift in organizational values, particularly around risk.
As healthcare industry professionals, we must equip practices with adequate support and resources to help them manage this risk effectively. Technology that provides patient access to their health information, real-time data insights, and personalized health care plans to help manage social determinants of health (SDOH) and chronic conditions using customized templates, machine learning or generative AI analytics are places to start and activities to watch.
Moving Forward: Strategies for VBC success suggested by survey insights
- Education and Support: It’s critical for healthcare administrators, practice managers, and physicians to learn about the benefits of VBC and be able to access resources that assist in transitioning to these models. Workshops and training sessions can demystify VBC, addressing concerns and building confidence, and a strong healthcare IT partner is critical to ensure the data infrastructure, reporting capabilities and cohort management functionality is embedded into clinical workflows. Better yet, a partnership with a comprehensive EHR, practice and revenue cycle management and patient engagement HIT vendor such as athenahealth includes training and support from customer success managers as well as access to a robust support community enabling physicians to learn from each other.
- Enhancing Interoperability: Investing in interoperability between EHR systems can streamline workflows, reduce administrative burdens, and facilitate the delivery of high-quality care. Interoperable systems that provide a clearer, more holistic picture of a patient’s health are critical to the care coordination, health outcomes, and controlled costs metrics within VBC programs. Clinicians using athenaOne® become part of athenahealth’s nationwide cloud-based network, have automatic connectivity to tens of thousands of other providers through managed partnerships, and access to over 165k other clinical integrations.5
- Fostering a Culture of Innovation: Encouraging the adoption of AI and other technologies can improve operational efficiency and patient outcomes, making practices more competitive in a value-based landscape. Automated solutions that use Natural Language Processing to parse incoming healthcare reports and assign them to the appropriate patient health record are critical to streamlined workflows and to serving the right information at the right time during the patient encounter so physicians can uncover and manage the care gaps and health outcomes that are critical to VBC. AI innovations in EHRs such as Ambient Listening to automate physician notes from a patient encounter also show promise in ensuring accurate and complete health data is captured and documented for VBC reporting and improved healthcare outcomes.
- Risk Management Tools: Providing practices with tools to assess and manage financial risks associated with VBC can alleviate some of the anxiety surrounding these models. In comprehensive EHR, practice and revenue cycle management and patient engagement software solutions such as athenaOne, robust reporting dashboards for VBC metrics, at-a-glance reports for payer reimbursements, and patient engagement tools that help with outreach and adherence to care plans can all help with these efforts to lower upside and downside risks. Additionally, some research has shown that diversifying payment models with a mix of FFS and VBC helps practices feel more financially secure.
Keeping the pulse on value-based care needs as 2030 approaches
The transition to value-based care represents both a challenge and an opportunity for physicians and healthcare administrators alike. By understanding the sentiments of physicians and addressing their concerns through education, improved systems, and supportive technologies, we can help pave the way for a more sustainable and efficient healthcare ecosystem and meet the regulatory demands as the 2030 CMS goal of 100% of Medicare beneficiaries on value-based care approaches. As we move forward, collaboration between healthcare providers, facilities, and technology partners will be key in ensuring that all stakeholders thrive in this new paradigm of care delivery.
More implementing VBC resources
Continue exploring
- Person-Centered Innovation – An Update on the Implementation of the CMS Innovation Center’s Strategy November 2022
- https://www.cms.gov/priorities/innovation/data-and-reports/2022/cmmi-strategy-refresh-imp-report
2023 Physician Sentiment Survey of 1,003 physicians nationwide, commissioned by athenahealth and fielded by Harris Poll, Jan 2024. Metrics noted in this article are sourced from the 2023 Physician Sentiment Survey unless otherwise noted. - "Substantial" was defined as physicians who responded "a lot" or "almost all" to the following question: To what extent is your practice or organization bearing financial risk (i.e., adopting value-based care models where payment is tied to results delivered, such as quality, equity or cost of care) for your patient population?
- The 11.5% of FFS physicians who reported a financial risk may have misinterpreted the survey question and wrongly indicated that they are sharing risk or did not realize they are VBC.
- Based on athenahealth data as of Dec. 2023; M020








