How direct integration with athenahealth eliminates the need for manual chart retrieval and improves data accuracy in real time
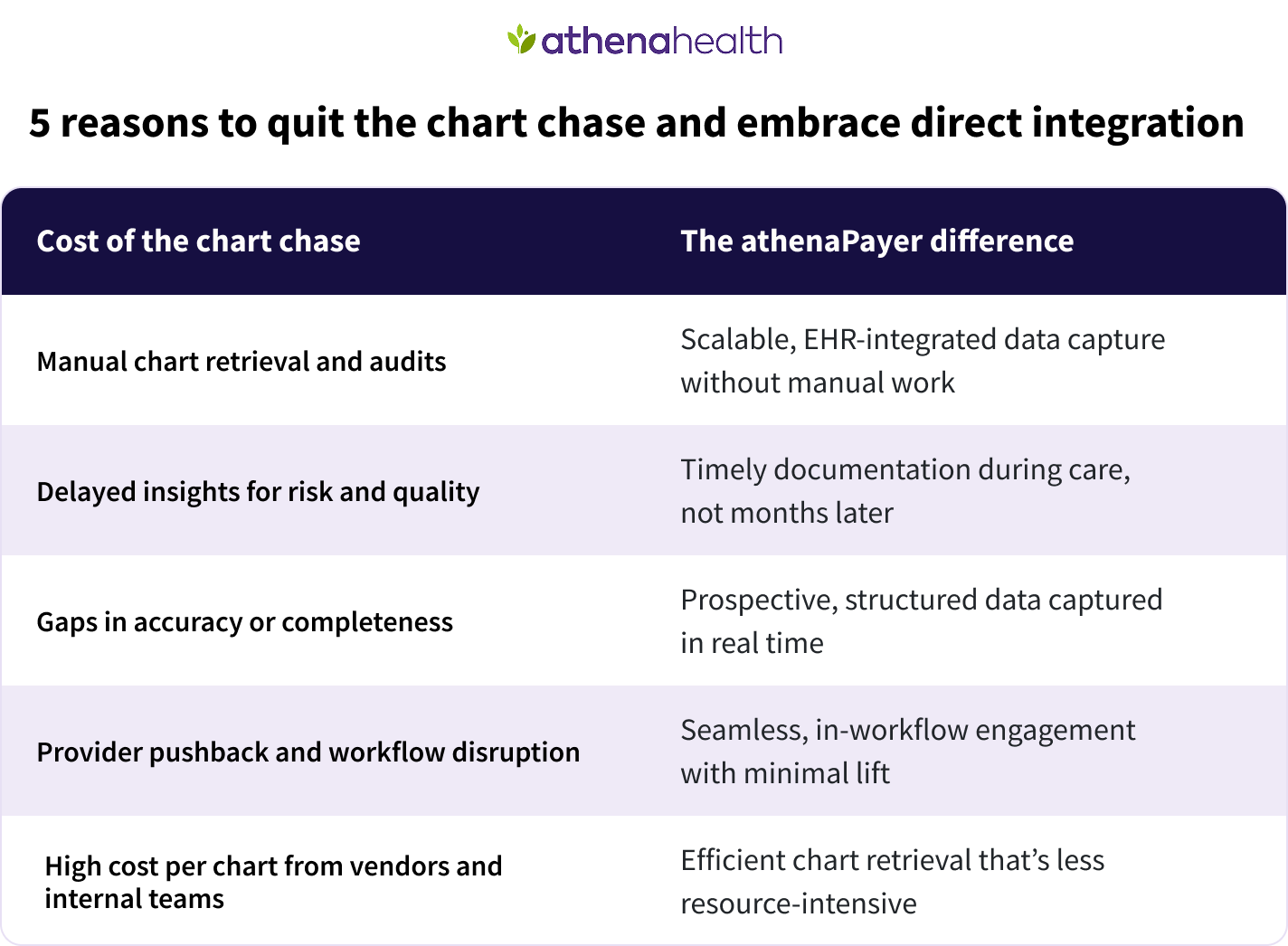
Chart chasing remains one of the most resource-intensive and delay-prone processes in payer operations. The entire experience is fraught with challenges: labor-intensive manual outreach to providers, inconsistent record formats, and retrospective review that often happens long after the moment of care. What's more, despite the effort and cost spent on retrieving essential member information, this type of manual chart retrieval still results in gaps in diagnosis capture, delayed quality reporting, and increased provider abrasion. It’s disruptive to practices — and expensive for payers.
athenaPayer offers a better model. Through connection with athenahealth’s nationwide network of 170K+ providers1 across all 50 states, payers gain real-time integration with clinical workflows — without needing to enroll individual providers, one at a time. Payers’ insights about their members are embedded directly into the provider’s EHR at the point of care, so critical information is captured prospectively, and chart chases become largely unnecessary.
For speed, efficiency, and convenience, direct integration outstrips manual chart retrieval:
- Eliminates the need for most retrospective chart pulls and audits
- Enables real-time, structured documentation aligned with risk and quality programs
- Provides insights for Stars, HEDIS, and RAF forecasting
- Reduces provider fatigue and streamlines payer operations at scale
Enable prospective risk and quality capture
Rather than chasing documentation months after the visit, athenaPayer allows payers to surface open care gaps, suspected conditions, and documentation reminders in the EHR while the member is still with the provider. This proactive approach supports timely and complete capture of clinical data — right when it’s most actionable.
With proactive information, payers can gain enormous benefits:
- Enhances the accuracy and completeness of risk adjustment coding
- Improves care gap closure rates for Stars and HEDIS
- Gives quality and actuarial teams earlier visibility into performance trends
- Reduces reliance on vendor-led or manual chart reviews
Reduce cost and complexity across your clinical data operations
Chart chasing is not just expensive, it’s operationally complex. It requires coordination across teams, vendors, and provider systems, often with incomplete or unstructured results. athenaPayer simplifies this process by embedding documentation tools within the workflows of providers already using athenahealth — eliminating manual handoffs and accelerating data availability.
Meet your goals with the right data, captured with simplicity:
- Lower overall cost of data acquisition for risk and quality programs
- More complete and audit-ready documentation, captured at the source
- Fewer touchpoints, fewer errors, and faster turnaround times
- Scalable infrastructure that meets performance and compliance goals
athenaPayer embeds documentation tools within the workflows of providers already using athenahealth — eliminating manual handoffs and accelerating data availability.
Strengthen provider relationships by removing administrative burden
Accommodating chart requests can be a headache for provider organizations. These on-site chart chases divert clinical resources away from patient care and can be disruptive to the practice — especially when it’s duplicative across lines of business. By minimizing or even eliminating the need for chart chases, athenaPayer improves payer-provider alignment and makes value-based collaboration more sustainable.
Build more harmonious relationships that benefit payers and providers alike:
- Less frustration and workload for provider staff
- Fewer redundant requests across plans, contracts, and teams
- Stronger provider engagement in risk and quality programs
- Greater satisfaction in shared performance initiatives
Ready to stop chart chasing and start exchanging data in real time?
Chart chasing, faxed records, and post-service audits are holdovers from a fragmented era of healthcare. For payers investing in value-based performance, real-time data, and collaborative provider relationships, these legacy workflows have become unsustainable.
athenaPayer provides a modern alternative: a single connection that delivers embedded, real-time access to 170K+ providers across the country, automatically, with no individual opt-in required. This is infrastructure built for scale, speed, and actionable insight.
Whether your goals include reducing administrative burden, improving risk accuracy, accelerating quality performance, or lowering total cost of data operations, athenaPayer gives you a simpler path forward.
Lead your organization into the future... and leave the chart chase in the past.
Let's talk about how you can reach your goals with athenaPayer. We’re happy to share:
- Comparative data quality and timeliness benchmarks
- Case studies from national and regional plans
- Integration timelines and technical documentation
- Cross-functional benefits for risk, quality, claims, actuarial, and network teams
Read more about athenaPayer, then connect directly with our payer partnerships team to schedule a conversation.
More payer solutions resources
Continue exploring
- Based on athenahealth data as of Sept. 2025; M010










