Boost efficiency with authorization management solutions
Authorization solutions for athenaOne®
Empower your staff with tools to streamline authorizations, or let us work them to completion on your behalf with our fully embedded authorization solutions.
Find the authorization solution that’s right for your organization
Hand authorization work off to our specialists with athenaOne Authorization Management, or enable your own team to unlock new efficiencies with Express Authorizations. Both solutions are fully integrated within your existing clinical workflows.
Express Authorizations
Improve efficiency with intuitive authorization and referral workflows.
Authorization Management
Let athenahealth’s expert teams take on most authorization work for you.
Express Authorizations
Intelligent automations and intuitive workflows
Streamline authorization work with native tools and technology that enable staff and clinicians to access relevant details and tasks within their existing workflows.
Reduce authorization work
Spend less time on and avoid submitting unnecessary authorizations with our automated Authorization Determination Engine.
Unblock patient access
Monitor authorization status at a glance with our Authorization Tracker, ensuring timely follow-up and expediting patient care.
Drive higher-quality outcomes
Minimize inaccurate or incomplete requests with up-to-date payer requirements that eliminate the need for rules lists and constant research.
athenaOne Authorization Management
Alleviate authorization work
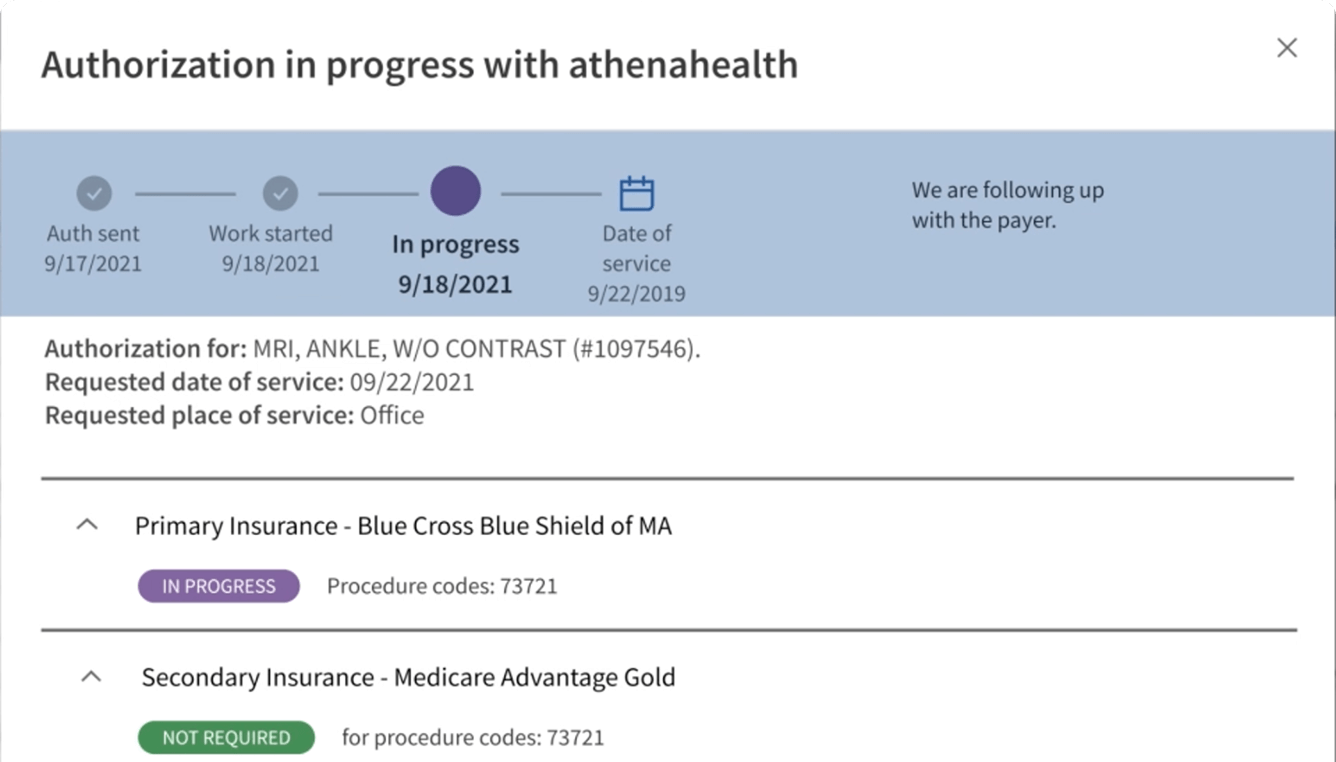
When you submit an eligible order, our Authorization Determination Engine checks it against payer regulations. If authorization is needed, our specialists communicate with payers to submit documentation, follow up on status, and manage it to completion.
Stay compliant with payer requirements
Save the time of tracking changes across payers. Our determination engine and authorization processes are continuously updated with the latest requirements and monitored for accuracy.
Enable timely authorizations
Authorization specialists work around-the-clock to keep your appointments and patients on track.
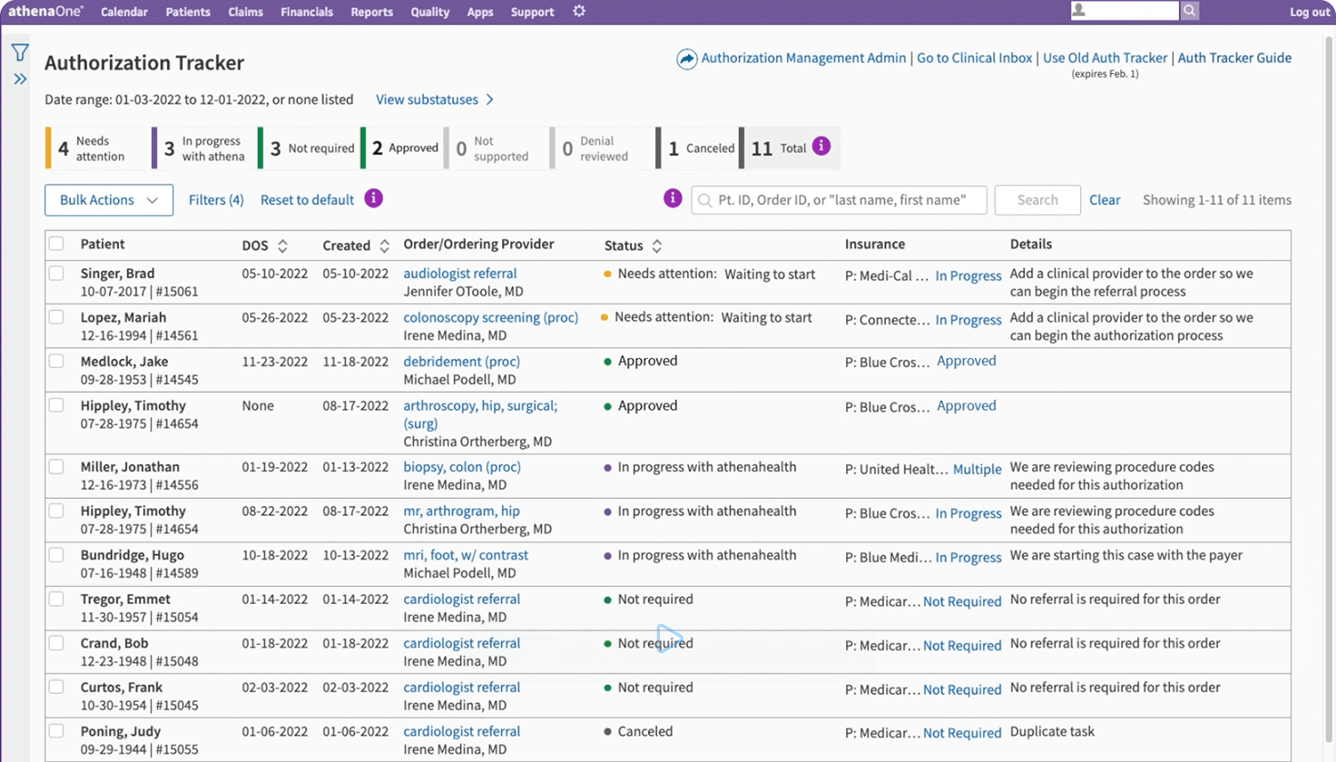
Maintain complete visibility
Track the process and the status of your medical authorizations at any time with the Authorization Tracker dashboard. View details of individual cases and communicate with our specialists as needed.








