Revisiting the promise of AI for clinical diagnoses
In 2018, artificial intelligence in healthcare seemed poised for a moonshot. Watson had already conquered Jeopardy!, and IBM’s partnership with MD Anderson Cancer Center to fight cancer symbolized what many hoped would be AI’s inevitable clinical breakthrough. “In the future, AI will benefit patients. But today it can help doctors,” said Girish Venkatachaliah, former VP of Watson Machine Learning and then vice president of data strategy, analytics and machine learning at athenahealth.
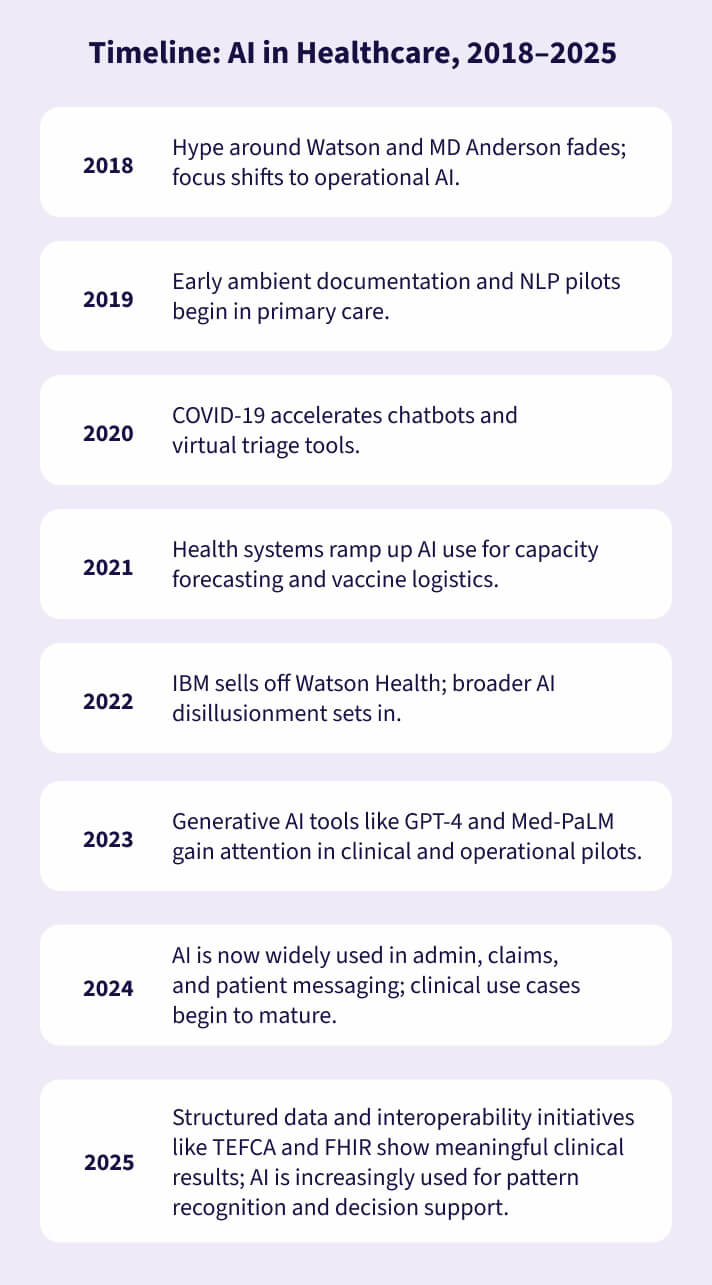
But seven years later, in 2025, has AI lived up to that promise?
2018 vs. 2025: AI’s role in healthcare reality check
Despite the general market hype in 2018, MD Anderson discontinued its high-profile partnership with Watson. By 2022, IBM had sold Watson Health to private equity firm Francisco Partners, acknowledging the difficulty in turning AI’s potential into sustainable clinical products. The nuances of medicine, with its often unstructured, incomplete, and context-sensitive data and important privacy restrictions, can make it harder to obtain the large data sets needed to train artificial intelligence. That, in turn, has limited AI’s ability to provide clinical decision support.
Meanwhile, operational AI in healthcare has quietly flourished. The past seven years have seen a boom in applications that reduce administrative burden, with athenahealth continuing to help pioneer new avenues for improving clinical workflows – a process that launched under Venkatachaliah’s lead with using AI to revolutionize incoming fax processing for medical practices.
Seven years of AI innovation: How athenahealth revolutionized fax workflows with machine learning
In 2018, long before the current wave of AI hype, athenahealth recognized healthcare’s greatest challenge wasn’t a lack of clinical expertise; it was inefficiency. Physicians and staff were drowning in administrative work, especially when it came to processing the millions of faxes flowing through medical practices every year – individual documents related topatient information that had to be sorted, digitized, and connected to a patient record.
athenahealth research from 2018 found that each fax took over two minutes to review and manually enter into patient records, adding up to roughly 200 hours of wasted administrative time per provider each year and contributing to the $190 billion in administrative waste burdening U.S. healthcare, a 2018 number that has now ballooned to $440 billion annually, according to the 2024 CAQH Index® Report.
Led by Venkatachaliah’s team, athenahealth became the first EHR vendor to use AI to solve information overload and administrative bloat. In 2018, the company launched an AI-driven approach to transform the manual, analog fax process into a streamlined digital workflow. By combining machine learning, cloud computing, and seamless EHR integration, athenahealth’s solution became the industry’s first scalable, AI-powered fax management system.
Over the past seven years, this AI-powered document services innovation has evolved across the athenaOne® network, delivering:
- AI-assisted data extraction – Machine learning scans incoming faxes, identifies critical document details and can automatically put the document in the right patient’s chart and assign it to the right user for review.
- Massive efficiency gains – What once took more than a minute per fax now takes under 30 seconds, saving hundreds of hours per clinician each year.
- Error reduction & data integrity – Automated processing leads to fewer mistakes, improving the quality of records and analytics.
- Lower clinician burnout – By reducing tedious administrative work, AI frees providers to focus on patient care, helping to combat the burnout linked to time-consuming documentation
Today, athenahealth continues to build on this foundation of AI innovation with smarter automation, more structured data transformation, and seamless cloud faxing via integrating eFax Corporate Cloud Solutions directly into the athenaOne platform. What started as a way to digitize faxes transformed due to AI into a full data pipeline, turning healthcare’s most outdated workflows into a driver of speed, accuracy, and cost savings across the care continuum.
As the ecosystem matures, AI is beginning to live up to its potential: reading test results, flagging high-risk patterns across specialties, and helping clinicians spot risks sooner.
Where AI has delivered in the healthcare industry
AI has quietly become indispensable for small practices and large healthcare organizations alike in these areas:
- Administrative efficiency: AI-assisted fax routing, prior authorization prediction, and ambient documentation tools save clinicians minutes per task—which adds up to hours per week.
- Revenue cycle optimization: Machine learning is widely used in claims scrubbing, coding support, and denial prediction.
- Patient engagement: Chatbots, automated reminders, and even AI-generated follow-ups now support millions of patient interactions.
These tools succeed because they solve small, well-scoped problems using structured inputs and predictable output.
What’s changed in healthcare AI since 2018: Generative AI is the headline, but not the whole story
Since 2023, generative AI tools like GPT-4 and Med-PaLM have sparked a new wave of optimism about AI’s possibilities in healthcare. These tools are more flexible, more language-aware, and capable of summarizing, drafting, and even reasoning. Health systems are piloting these tools for ambient notetaking, patient communication, denials management, and task triage.
athenahealth’s Ambient Notes, for example, uses generative AI technology and ambient listening to record patient visits and create a clinical note summary, leaving clinicians free to focus on patients. One physician called it “transformative” — simplifying clinical documentation, speeding her chart closure, and even improving billing accuracy.
Still, trust, transparency, and regulation remain major hurdles for generative AI. Other AI-powered innovations working more quietly in the background of the healthcare IT stack may be the biggest gamechangers, even if they don’t have as much hype.
The healthcare AI development journey: Real progress, grounded expectations
At athenahealth, we’ve seen the potential of AI since rolling out machine learning solutions for fax processing back in 2018.
Larger AI implementation has helped relieve some of the administrative drag that pulls clinicians away from care. Standardization and model evolution have also helped improve data sharing and brought about a new understanding of what interoperability really means. The buck does not stop there.
Continued AI optimization and maturation is unlocking even more clinical possibilities. Generative AI enhances healthcare interoperability by intelligently summarizing, standardizing, and structuring vast amounts of clinical data from disparate sources, making it easily comprehensible and usable for clinicians. Agentic AI, a form of artificial intelligence capable of autonomous decision-making and task execution, has the potential to further reduce clinical administrative burden.
The most powerful thing AI can do is still what Venkatachaliah said in 2018: “Do the jobs humans shouldn’t.” Machines, not humans, should be parsing mountains of data. That’s the promise of AI. While the story of AI in healthcare is still unfolding, its real impact is already clear: freeing clinicians from repetitive tasks, cutting through information overload, and fighting burnout. It hasn’t cured cancer, but AI may yet help fix healthcare.
“At athenahealth, our commitment to supporting our customers fuels our drive to transform healthcare through AI that delivers truly differentiated outcomes. From automating fax workflows to ensuring clinicians have the right information at the right time, we lead with solutions that reduce administrative burdens and empower clinicians to focus on what matters most—patient care,” says Alicia Bassolino, VP, Analytics and AI, at athenahealth. “As AI continues to evolve, we remain dedicated to pushing boundaries and delivering practical, impactful technologies that shape the future of healthcare.”
Learn more about how athenahealth is developing new applications for AI in healthcare.








