Advances in healthcare technology, interoperability of electronic health records, and other healthcare regulations have led to an explosion of information about every patient. Having more data points to analyze could be helpful in diagnosing, planning, and assessing treatment efficacy, but physicians are feeling the pinch of trying to sort, retrieve, and process all this healthcare data.
Physicians often attribute data overload to increased regulatory requirements, but they also cite issues with the usability and interoperability of electronic medical records. Together, these issues around too much information and not having the right information when they need it are contributing to physician burnout.
The latest athenahealth Physician Sentiment Survey identifies information overload as a major theme impacting doctors’ daily workflows, career satisfaction, and ability to do their jobs. Continue reading to learn more about what physicians had to say about note bloat, healthcare information quality and quantity, and how EHR systems use and display healthcare data.
Information overload in healthcare is an issue
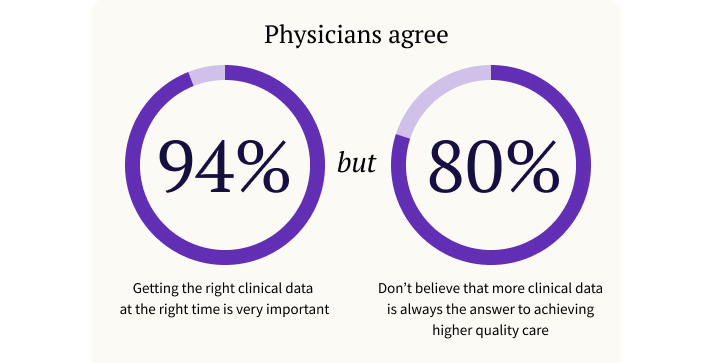
Roughly 1000 physicians nationwide felt strongly about information overload: 94 percent of respondents agreed that getting the right clinical data at the right time is very important to helping them do their jobs. Physicians overwhelmingly feel that accurate and timely information is critical to providing quality healthcare.
But how does streamlined, efficient information improve doctors’ clinical workflows? The right healthcare information when they need it helps reduce physician time spent reading, processing, and entering information into health charts and provides important data points to help the physician make a clinical decision. These, in turn, can improve job satisfaction, patient safety and healthcare outcomes.
Addressing data overload and EHR usability challenges with more efficient EHR workflows, better filters and templates to organize information, and seamless connections between EHR systems are all top priorities for athenahealth and the healthcare industry to address information overload and physician burnout.
Healthcare data overload increases physician stress and burnout
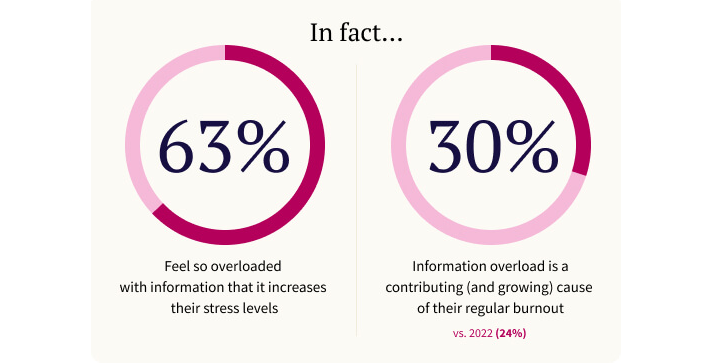
Roughly 80 percent of doctors reported in the most recent Physician Sentiment Survey that more data isn’t the answer in achieving higher quality healthcare. In fact, 63 percent of physicians stated that they feel so overloaded with information that it increases their stress levels.
Debate in healthcare about the best, most efficient kinds of patient notes for electronic health records continues, but provider notes are only one type of data in EHR systems. Electronic Health Records bring in information from other providers, as well as lab values, alerts, and patient communication.
There is more data than ever available to providers to make observations and decisions about a patient’s health indicators, but if that data isn’t useful or findable when the physician needs it, then it isn’t helpful. In fact, survey findings indicate that more data is worse for healthcare providers if it makes doing their job harder and less efficient.
It's the quality of clinical data that matters.
“Note bloat” or extraneous EHR information concerns are increasing
Around 30 percent of survey respondents specifically identified information overload as a contributing and growing cause of physician burnout. More concerning, perhaps, is the fact that this number is 20 percent larger than in 2022, when 24% of respondents cited information overload as a leading cause of their burnout.
Information overload concerns trending higher is the wrong direction for improving healthcare efficiency and reducing provider burnout. Multiple research studies echo the concerns in the Physician Sentiment Survey that there is too much data or the wrong kind of data at the wrong time in healthcare records.
For example, a comprehensive study of 28 peer-reviewed articles on information overload in healthcare identified a repeated complaint from doctors: extraneous information in electronic health care records, also known as “note bloat,” adversely affects EHR usability and increases physician workload.1
In addition to frustrating healthcare providers and contributing to physician burnout, study data also revealed concerns with cognitive overload and comprehension as physicians attempt to locate, filter and process so much data quickly, which could lead to errors and patient safety issues.
Physicians feel less prepared for patient encounters
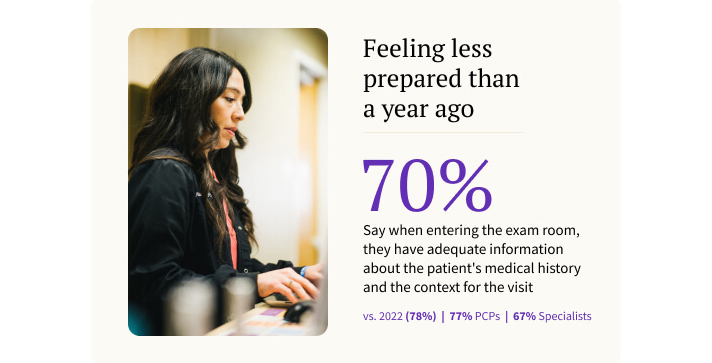
Another bellwether from the Physician Sentiment Survey is the number of physicians who say they feel prepared for a patient visit versus one year ago. Based on the latest research findings, this statistic is trending downward, with more physicians feeling unprepared when they enter an examination room year over year.
In 2022, 78% of physicians felt they had adequate information and context about a patient and their condition before starting a patient encounter, but that number is down to 70% in the 2023 survey.
Physicians want information delivered before and during a patient encounter, so they are prepared with a patient’s history and current health indicators at the point of care. Doctors are time-pressed as they move from patient to patient during a busy day and need to be able to locate and skim relevant information quickly to be ready for each new encounter. Information overload and EHR usability issues can make this more difficult than it ought to be.
Having relevant information available when they are talking to the patient helps improve the quality of care, clinical decision-making, and patient satisfaction. According to the Physician Sentiment Survey, doctors feel inundated by the sheer volume of information in EHRs and simultaneously feel they don’t have access to the info that they truly need, when they need it.
These findings on the Physician Sentiment Survey are confirmed in recent studies from the American Medical Association2, the Journal of Patient Safety, and others. To combat data overload, electronic health records need to give healthcare providers the information they need, at workflow appropriate timing, in a readable and intuitive manner, in a place they can readily find it.
Better EHR usability for higher quality patient care
We asked physicians about solutions that would have the greatest impact on their ability to provide higher quality patient care, and doctors again homed in on data efficiency, usability, and timely delivery of appropriate information.
Roughly 44 percent of respondents to the Physician Sentiment Survey said that the ability to find clinical data more easily when they need it was their top pick for improving their ability to provide better patient care. Doctors prioritize getting the right information at the right time as an important factor in improving both patient outcomes and reducing their burnout.
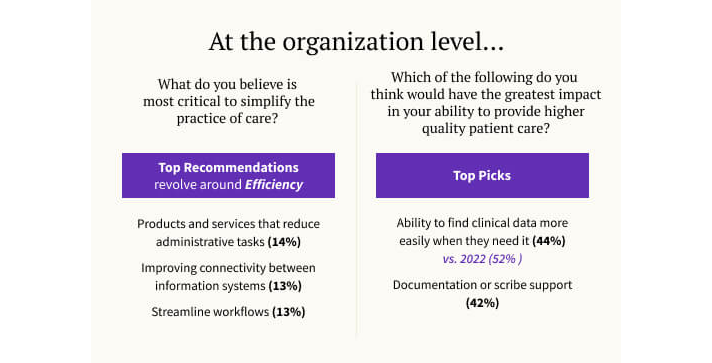
A second top pick to improve patient care that doctors identified is EHR documentation or scribe support (42% of respondents) to reduce the time spent updating health records and helping ensure consistency with data input.
With both ways to improve their day-to-day clinical experiences related to information overload in healthcare, it’s evident that providers need solutions – either with technology or services – to help make their jobs easier, more efficient, and better for patients as well.
EHR interoperability issues contribute to data overload
According to the Physician Sentiment Survey, 64 percent of respondents felt frustrated by the challenges of accessing clinical information about their patients from other providers. Linking healthcare data about a patient from one doctor, clinic, hospital, lab, pharmacy, or ambulatory care center is the core of interoperability and meaningful use of EHRs regulations implemented in the last decade by the Centers for Medicare and Medicaid Services (CMS).
But even with all the regulatory changes requiring interoperability of EHR systems, physicians continue to loudly voice problems with information overload and data usability.
It's not enough to simply get different electronic health records systems to talk to each other and share data. Being able to exchange data with another EHR may comply with the letter of the law, but that doesn’t mean that all EHRs are presenting information in a usable, relevant, and curated way, which is the spirit of the law.
As physicians clearly identified in the Physician Sentiment Survey, they want and need an EHR to display imported information in an intuitive and integrated manner. Improving this information exchange and user interface – in other words, true interoperability – would reduce physicians’ frustration and boost the quality of care, according to nearly two-thirds of survey respondents.
More about the state of healthcare in America, according to doctors
Doctors’ concerns about information overload in healthcare is only the tip of the iceberg of important data points in the latest athenahealth Physicians Sentiment Survey. These other articles take a closer look into topics surfaced in the research:
- Excessive clinical documentation and whether AI can help
- Managing patient communication demands
- Medical Practice financial stability and payment models
- Managing changing and challenging government healthcare regulations
- Simplifying clinical workflows and easing administrative burden
- Healthcare staff turnover, doctors quitting and nurses leaving
Customized EHR workflows and templates for your practice
Electronic Health Records and clinical practice management software can’t be a one-size-fits-all-solution, as physicians have clearly noted in the Physician Sentiment Survey. Customized templates that surface and display relevant patient information at the right time in your workflow is critical, as is filtering out extra information you don’t want to sift through to find what you need.
Curing complexity is our goal as we build a networked, integrated, provider-centered, practice-management ecosystem that delivers high-quality, accessible, and sustainable healthcare for all. We’ve invested over $730 million in the past 3 years on R&D to drive improvements in feature functionality, reliability, and supportability.3
Talk with an athenahealth solutions representative for your practice specialty and learn more about how our platform and services can help ease information overload in your daily workflows.
Read the updated 2025 Physician Sentiment Survey report.
More data overload resources
Continue exploring
References
Arnold M, Goldschmitt M, Rigotti T. Dealing with information overload: a comprehensive review. Front Psychol. 2023 Jun 21;14:1122200. doi: 10.3389/fpsyg.2023.1122200. PMID: 37416535; PMCID: PMC10322198. Dealing with information overload: a comprehensive review - PMC (nih.gov)
Athenahealth, Physicians’ Sentiment Survey. Survey, commissioned by athenahealth and fielded by Harris Poll, Jan 2024.
Furlow, Bryant. Information Overload and Unsustainable Workloads in the Era of Electronic Health Records. The Lancet: Respiratory Medicine. Volume 8, Issue 3, P 243-244. March 2020. DOI: https://doi.org/10.1016/S2213-2600(20)30010-2
Howe JL, Adams KT, Hettinger AZ, Ratwani RM. Electronic Health Record Usability Issues and Potential Contribution to Patient Harm. JAMA. 2018;319(12):1276–1278. doi:10.1001/jama.2018.1171 Electronic Health Record Usability Issues and Potential Contribution to Patient Harm | Electronic Health Records | JAMA | JAMA Network
Kutney-Lee A, Brooks Carthon M, Sloane DM, Bowles KH, McHugh MD, Aiken LH. Electronic Health Record Usability: Associations with Nurse and Patient Outcomes in Hospitals. Med Care. 2021 Jul 1;59(7):625-631. doi: 10.1097/MLR.0000000000001536. PMID: 33797506; PMCID: PMC8187272. Electronic Health Record Usability: Associations with Nurse and Patient Outcomes in Hospitals - PMC (nih.gov)
Christine Sinsky, Lacey Colligan, Ling Li, et al. Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties. Ann Intern Med.2016;165:753-760. [Epub 6 September 2016]. doi:10.7326/M16-0961
- Nijor S, Rallis G, Lad N, Gokcen E. Patient Safety Issues from Information Overload in Electronic Medical Records. J Patient Saf. 2022 Sep 1;18(6):e999-e1003. doi: 10.1097/PTS.0000000000001002. Epub 2022 Apr 7. PMID: 35985047; PMCID: PMC9422765. Patient Safety Issues from Information Overload in Electronic Medical Records - PMC (nih.gov)
- Henry, Tanya Albert. 7 EHR usability, safety challenges—and how to overcome them. American Medical Association. 2023, December 11. 7 EHR usability, safety challenges—and how to overcome them | American Medical Association (ama-assn.org)
- Based on athenahealth data, cumulative investment over three years ending Dec. 2023; M166











