Population Health Management for VBC Success
Solutions for the right care at the right time
Coordinate care across your entire patient community with our population health management tools, native to athenaOne®.

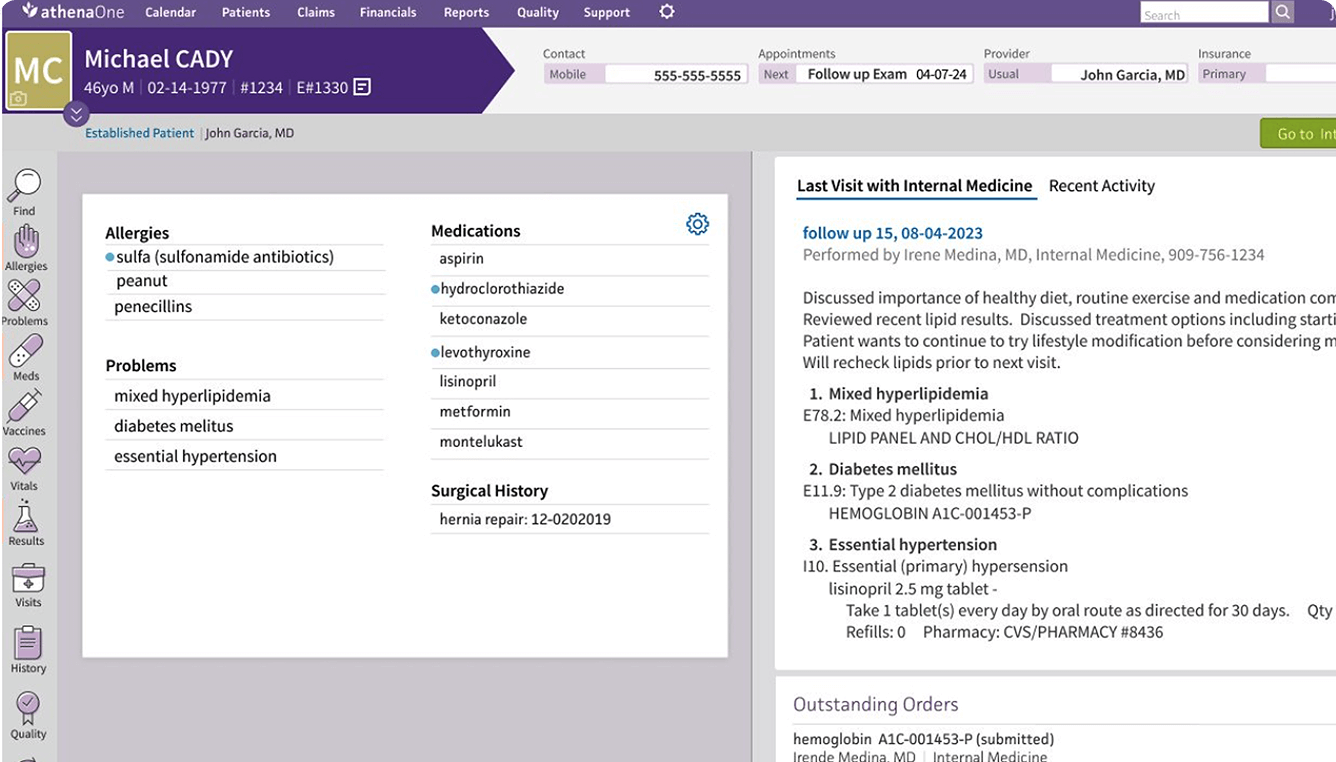
Get the data you need to manage your population
Simplify care coordination and engage patients wherever on the risk spectrum your organization falls. Our population health tools are native to athenaOne and surface the right data at the right time to improve outcomes.
Streamline care coordination
Provide the right care at the right time using data incorporated from across the healthcare ecosystem and surfaced directly in your clinical workflows.

Close care and diagnosis gaps
Make it easier to address care and diagnosis gaps with alerts surfaced directly in the patient chart and automated outreach services to keep patients engaged.
Enhance care program visibility
Quickly identify which patients are enrolled in care programs to deliver targeted care and improve financial outcomes with athenaOne’s care program panel.
Ease the burden of VBC
See which patients have successfully satisfied care gaps to streamline value-based care reporting for quality programs and HEDIS® with our Data Explorer.1
Coming Soon: Population Intelligence for athenaOne
Leverage population-level data for value-based care success
With athenaOne’s upcoming Population Intelligence add-on, clinicians will be given access to enhanced data and insights through native analytics tools at the point of care. This will provide support to close care and diagnosis gaps faster and improve patient outcomes, quality metrics and cost.
Simplify data management across your organization
Improve staff efficiency with tailored, real-time insights based on data from payers, hospital notifications and a diversity of other clinical sources.
Unlock advanced population-level analytics
Optimize financial outcomes with the ability to measure organizational performance on a wider variety of quality metrics.
Enable enterprise-level care management
Empower staff to coordinate and document patient care across multiple EHRs using athenaOne’s care management platform.
Drive even more VBC success
Explore multiple ways to alleviate the burdens of value-based care reporting, including ACO support, with fully-integrated Marketplace solutions.
Frequently Asked Questions
How do athenaOne’s native tools help support value-based care contracts and risk-based arrangements?
athenaOne features extensive tools that support our customers regardless of where they are in their value-based care journey. From Day One, its native capabilities can help customers with the following:
- Predict and identify patients who need care
- Engage patients so they schedule necessary appointments
- Deliver essential care while addressing any open care and diagnosis gaps
- Coordinate care through native care management and referral management tools
- Measure performance in valued-based programs using certified eCQMs, HEDIS® measures, and more1
Will Population Intelligence provide predictive analytics to help identify rising-risk patients early?
Yes, the Population Intelligence add-on will feature more robust data analytics. Organizations managing risk for large populations will be able to identify their most at-risk patients, as well as patients with rising levels of risk.
What types of data do athenaOne’s VBC tools ingest (claims, clinical, etc.)?
athenaOne natively ingests data from a variety of sources, including:
- Labs
- Imaging centers
- Pharmacies
- Vaccine registries
- Prescription drug monitoring programs
- HIE (including Carequality, Commonwell & the TEFCA framework)
- Payer and ACO partners
And more
athenaOne has the most connected network in healthcare, allowing it to serve up all of those connections and exchange relevant data to surface the right information for the right user at the right time. Population Intelligence will expand that existing connectivity by ingesting data from additional sources, including:
- Claims feeds
- Payer eligibility files
- Hospital discharge notifications
- Other EHRs
- Additional clinical data sources
What ROI can we expect from implementing athenaOne?
Each organization that implements athenaOne can expect to derive value differently based on the opportunities unique to their specialty and care model. athenaOne is designed to support customers by helping to reduce their most time-consuming work, freeing them to focus on higher priority tasks.
Customers can experience ROI as:
- Spending less time managing documents and more time with patients
- Better clinical outcomes due to having relevant information surfaced in their workflows
- Improved quality performance
If you are interested in learning how athenaOne could add value to your organization, click on the “Request a Demo” button to get a custom assessment.
Do you have case studies or resources that demonstrate how athenaOne helps organizations like mine?
We have several case studies and resources that speak to athenahealth’s investment in our customers’ success. Visit our Resource Center to learn more.
Can we expect to see improvements in quality metrics and cost reduction with athenaOne?
athenahealth clinicians consistently outperform the nation in 2023 MIPS and eCQM performance.
- 79.02% of eligible athenaOne providers achieved Positive Payment adjustments in Traditional MIPS PY2023, compared to 75.43% nationally*
- 72.09% of eligible athenaOne Orthopedic providers achieved positive payment in PY2023, compared to 58.53% nationally*
- 92.02% of eligible athenaOne Women’s Health providers achieved positive payment in PY2023, compared to 81.40% nationally*
- 84.51% of eligible athenaOne Cardiology providers achieved positive payment in PY2023, compared to 72.37% nationally*
Additionally, athenaOne primary care clinicians consistently received high ratings for measures included in the 2024 Medicare Advantage Stars program, including:
- 94% received four stars or greater for Medication Review as part of Care for Older Adults+
- 93% received four stars or greater for Statin Therapy for Patients with Cardiovascular Disease+
- 61% received four stars or greater for Controlling Blood Sugar as part of Diabetes Care (measure weight: 3x)+
- 57% received four stars or greater for Controlling Blood Pressure (measure weight: 3x)+
Continue exploring
1. The Healthcare Effectiveness Data and Information Set (HEDIS®) is a registered trademark of NCQA.
*Results from 2023 Quality Payment Program Experience Report (QPP – cms.gov).
+Results from athenahealth data for the listed performance periods Jan – Dec 2024.







