Delivering care is a joy when you've got a great team by your side – but many providers struggle with rigid job descriptions, a lack of resources, and cultural pressure to go it alone.
Solutions are within reach, though: New research from athenahealth reveals that empowered clinical teams limit administrative burden, lower burnout levels, and improve provider retention.
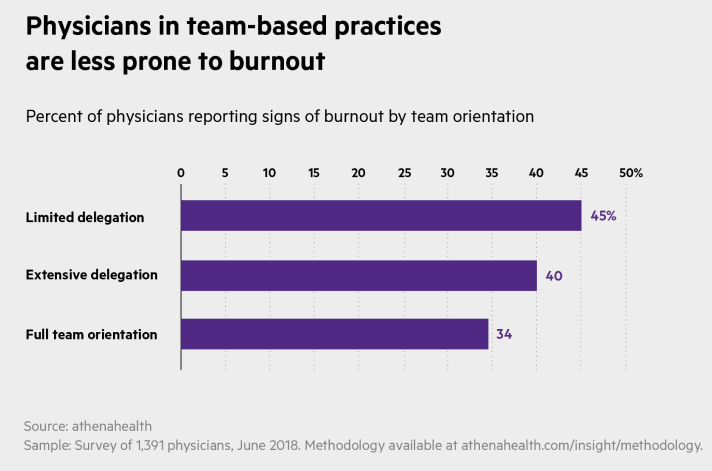
A group of 1,391 practicing physicians surveyed in June of 2018 were asked if they worked with limited delegation, extensive delegation, or a full team orientation. Those physicians with limited delegation were 32 percent more likely to report symptoms of burnout than those with a full team orientation. Extensive delegation helped a bit, but still lacked the impact of a close clinical team.
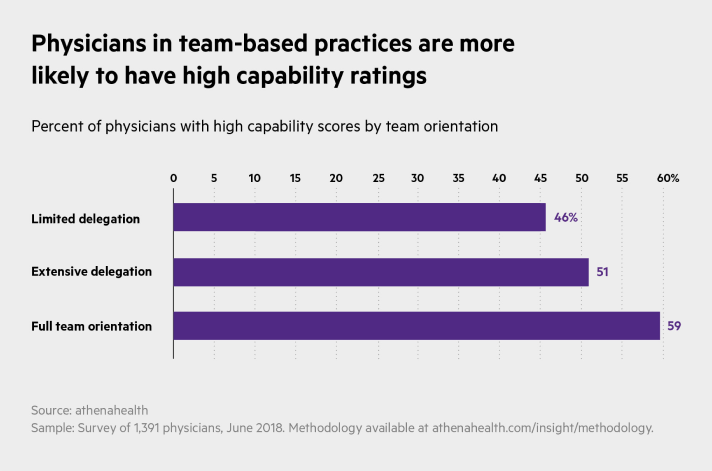
The data show that well-integrated clinical teams correlate with "capability" — that is, the measure of whether physicians have the tools, resources, and latitude to provide high-quality care to their patients. Fifty-nine percent of physicians who work in full team orientation have high capability scores, versus 51 percent who work in practices with extensive delegation and 46 percent with limited delegation.
The good news: Shifting to a team-oriented model doesn't have to be a heavy lift. Medical group leaders interviewed as part of the research suggest several tactics to make the transition. One thing they all have in common? Human connection.
Here's how to make the switch:
1. Break down inflexible roles
In a team-oriented practice, roles expand beyond their traditional boundaries.
At Valley Medical Group's four practices in Western Massachusetts, physician assistants work interchangeably with nurse practitioners. Moreover, each is partnered with a supervising physician, often even sharing an office.
This proximity, and the resulting close communication, means patients are able to see an informed provider quickly, even if it's not their primary practitioner.
After a while, according to Steven Esrick, M.D. at Valley Medical, patients accept the benefits of having a comprehensive care team. Patients especially welcome the flexibility — for instance, a patient with a male primary care doctor can choose a female PA for her gynecological exam.
Valley Medical has also expanded its medical assistants' usual role. They're not just taking vitals, but supporting quality management during Medicare annual wellness visits. The MAs can flag gaps in care and queue up care plans to close them.
And Valley Medical will soon be testing the benefits of assigning two MAs to one provider. Those MAs will add scribing to their duties, with the goal of lowering the physicians' documentation burden — leaving more time for care delivery.
2. Build teams from the get-go
At Mohawk Valley Health Systems, which has 21 primary care locations and several specialty centers in and around Utica, New York, providers learn a deep understanding of each other's patients and administrative needs, as well as the practice's cultural norms. And that indoctrination starts the moment they arrive.
Physicians new to the Mohawk Valley Endoscopy Center don't see their own patients until they've shadowed the other 10 physicians at the practice. Likewise, new midlevel providers shadow other midlevels — and only then move on to each physician. This “clinical watch period" includes regular journal clubs and other supplementary education.
By the time new providers start seeing their own patients, according to Bradley Sklar, M.D., medical director of Mohawk Valley Endoscopy Center, they have the practice's full confidence and plenty of institutional knowledge behind them.
The goal isn't just independence. This comprehensive onboarding ensures providers can cover each other at busy times and deliver faster care to patients. While physicians will meet their new patients on the first visit or medical event, afterward any Mohawk Valley provider can step in to keep care moving. “We try to make it so that it's more flexible," says Sklar.
And with monthly all-staff meetings to troubleshoot and compare notes, providers can easily keep each other in the loop.
3. Connect physicians with physicians
The hierarchical model of medicine keeps physicians at the top – but where can they turn when they need advice? The answer: other doctors.
Michael Harris, M.D., is one of 13 oncologists at MultiCare Regional Cancer Center in Puyallup, Washington. The organization holds weekly “tumor boards"— conference calls to discuss complex patient cases and compare perspectives. At monthly research meetings, providers also update each other on clinical trials, both to gauge interest and tackle logistical issues, Harris says.
The network now transcends meeting times. “Let's say I have a third line pancreatic cancer patient, and I don't really see a clinical trial nearby," says Harris. “What are my colleagues doing?"
After sending out an email, “Within an hour I get two or three messages back," Harris says. “They're telling me what they would do in that situation. And so at least by the end of the afternoon, when I'm likely to see that patient, I'll have some of my colleagues weighing in."
4. Invest in behavioral specialists
As providers are asked to manage broader patient needs in less time, they can benefit from having easy access to specialists for their patients. Ready access to social and behavioral specialists not only improves care delivery, but can ensure a provider covers patient needs that require more time.
“It's absolutely crucial," says Heidi Beery, M.D. at Evergreen Family Medicine in Roseburg, Oregon. Evergreen uses a Patient Centered Medical Home (PCMH) model, which integrates chronic care managers and mental health specialists into the care team.
This support team ensures consistent, quality care so patients who are wrestling with diabetes, congestive heart failure, and other chronic illnesses don't fall through the cracks. “Having that ability for them to come in and see the nurse, see that chronic care manager" is reassuring, says Beery. “I know that they'll be seen once a month."
A social worker on staff also provides invaluable — and immediate — support for primary care patients who turn out to also have behavioral health needs, increasing their likelihood of treatment. “On a typical day, I will have at least two, if not four or five patients where I need her to step in."
Empowered clinical teams require a practice-wide willingness to lower barriers and increase collegiality. The benefits pay off though — for providers as well as patients.
More reducing admin burden resources
Continue exploring
Alison Pereto is a staff writer for athenaInsight. Additional reporting by Payal Patnaik.












