How healthcare tech enhances patient and provider experiences
Virtual communication — portal messages, telehealth visits, text reminders — has become an integral part of patient-provider relationships. This trend was accelerated by the COVID-19 pandemic and shows no sign of returning to pre-pandemic norms; patients have come to expect the ability to hop on a same-day telehealth visit or to ask questions about their medication late at night through the portal.
Ever-increasing levels of provider and staff burnout and widespread staffing shortages due to the great resignation have made it imperative to leverage technology for automation when possible. Automation should be used for all the tasks that don’t really need a human touch, such as sending an automated “please remember to obtain your colonoscopy that Dr. Jessel ordered at your last visit” reminder. This first-pass outreach doesn’t need to be done in person — it just needs an algorithm to remind someone who hasn’t gotten around to scheduling. Instead, staff at the practice can focus on spending time with patients who are having second thoughts or have additional questions, potentially closing care gaps for patients who might not otherwise address them.
Appointment and prescription reminders, normal lab results — none of these require in-person communication. When used like this, automation doesn’t distract from the patient-provider relationship; rather, it adds to it because providers and staff have fewer administrative tasks on their to-do lists and can spend more time on high-value interactions during the all-too-short time they have with patients during appointments.
One of the things we learned during the pandemic is that many patients really prefer this kind of asynchronous communication — not just for reminders, but to get their questions answered. Before the pandemic, if a patient had a medical question, many practices would have told them to come in for an appointment. Because in-person visits were challenging or not possible for long stretches during the pandemic, offices widely adopted virtual care in the form of telehealth and electronic communication. As a result of this, many patients now expect to be able to ask medical questions electronically and have the provider answer it whenever they have the time. It’s like remote work — most of us don’t want to go back to the office full time.
Electronically resolving medical issues that would previously have required a visit can be better for both the patient and the provider — as long as providers are appropriately compensated for their expertise and time. athenahealth’s network data show that providers are spending more and more time resolving these more complex patient cases that take the place of in-person visits. In our current fee-for-service world, providers should be compensated for the time they spend furnishing their expertise outside of office visits — like other professionals who charge for the provision of their expertise in electronic form (think email exchange with lawyers). Expecting providers to provide these services for free and outside of regular office hours will continue to add to provider stress and burnout and ultimately affect patient care. Facilitating provider documentation of — and billing for — such asynchronous virtual patient care would protect this valuable communication and care delivery method and make it financially sustainable for practices.
Of course, ultimately these challenges will best be solved by moving to a more holistic healthcare system — in a fee-for-service world, keeping the patient out of the office and keeping them healthy doesn’t really pay off. Providers will still do it because it’s the right thing to do and they want the best outcomes for their patients. But I continue to believe that the ongoing transition from fee-for-service to value-based care models is the optimal way to align incentives for patients, payers, and providers and will accelerate the adoption of these communication strategies and tools.
Automated outreach can be an invaluable tool to explain health recommendations and gently nudge patient behavior. Like a text reminder to “pick up your prescription today” allows a patient to click on a link to learn more about the medication, we can visualize a future where these types of reminders could be extended to preventive services — such as mammograms, colonoscopies, or diabetic eye exams — helping close important care gaps. And these reminders could include statistics on why these screenings are so important and why they were ordered at this time. The truth is sometimes patients don’t feel comfortable asking questions during their appointments or don’t want to admit they really didn’t understand what the provider was talking about and why this is necessary. This kind of automated outreach, when done correctly, may serve to enhance health literacy and lay the foundation for shared decision-making.
And then, of course, the next logical step is to combine the reminder with the ability to actually schedule the primary care appointment right then and there — and, taking it a step further, link directly to labs and imaging facilities for scheduling, as well.
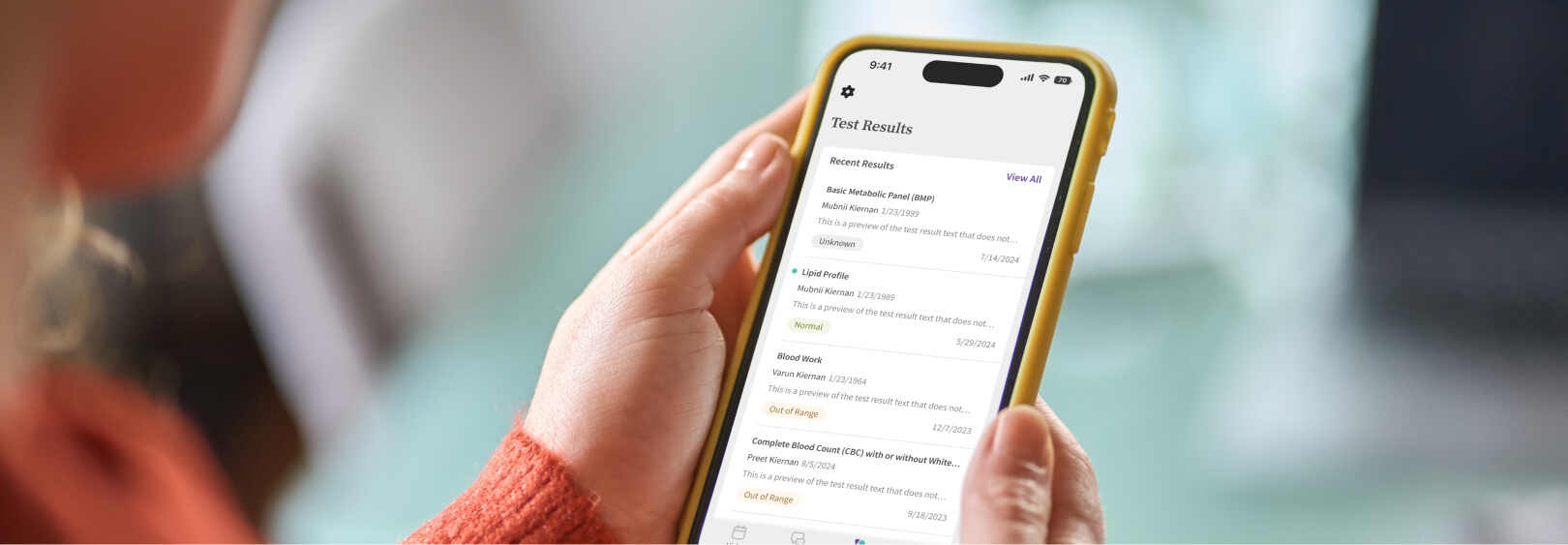
The real game changer will be patient apps that do all of this on a smartphone. Alerts and reminders will pop right up and link directly to the app. Lab and test results will be easier to review without logging into multiple portals. Both patients and providers can send messages while it is top of mind. And the smartphone really is the great equalizer, because almost everyone today has a one, even if they don’t have much else. Self-service on a phone app can be a great tool for reducing health disparities, especially when it is combined with surfacing health education.
And the more we reduce phone calls and shift communication to lower-effort channels, the more we free up providers and their staffs to focus on high-value interactions, support chronically ill patients, and provide more social supports and wraparound services. This will restore some much-needed professional enjoyment and help combat the ubiquitous provider and staff burnout we are seeing today. The key is to thoughtfully craft the patient experience of the future so technology augments or enhances the patient-provider relationship and doesn’t distract from it.
More patient communication resources
Continue exploring
Nele Jessel, M.D., is chief medical officer at athenahealth.












