Focusing on high-risk patients'social needs to close care gaps

The sickest patients who most need consistent preventive care often face systemic barriers to accessing care like mobility, lack of insurance, financial limitations, health literacy, and more. According to athenahealth data, the highest-risk patients — those with multiple chronic conditions — tend to be older than 60, and after adjusting for age, they’re disproportionately likely to live in a low-income zip code and to identify as Black or African American.
In early 2021, athenahealth began conducting research into how healthcare organizations engage and support these high-risk patients, those with two or more chronic conditions such as diabetes or heart disease. The research includes analysis of de-identified data from across athenahealth’s network of customers as well as conversations with clinicians and administrators. We found that addressing social determinants of health is a crucial part of caring for high-risk patients.
The gap between care needed and care received
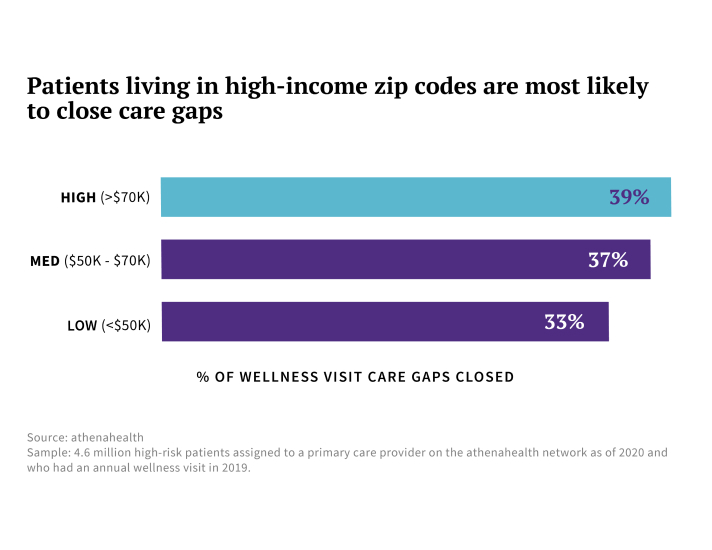
Socioeconomic status is a key determinant of how likely high-risk patients are to receive the care they need, like annual wellness visits. We looked at whether patients who had a wellness visit in 2019 returned for one in 2020, and then what percentage of those overdue patients ended up closing the care gap by scheduling a wellness visit within 90 days of their eligibility. The data show that wellness visit care gap closure rates increase alongside the socioeconomic status of patients’ neighborhoods.
Patients living in high-income zip codes — defined in the research as zip codes where the median household income is greater than $70k — were the most likely to close wellness visit care gaps that did arise. They closed 39% of care gaps within 90 days, compared with patients living in low-income zip codes, who closed just 33% of care gaps. Notably, patients of color had lower wellness visit care gap closure rates than white patients overall, but those differences went away after adjusting for income.
Patients living in low-income zip codes often struggle with other barriers to care, like lack of insurance or difficulty obtaining time off work for doctor’s appointments. That may help explain why the data also show a discrepancy between care gap closure at Federally Qualified Health Centers (FQHCs) versus non-FQHC organizations.
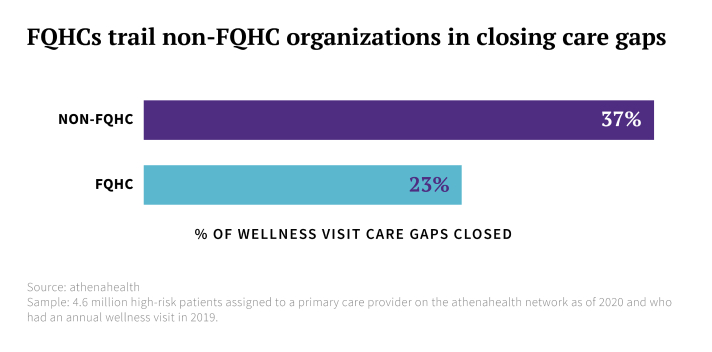
“As an FQHC, what we see is that for those patients that do identify any social determinant of health, it’s not just one factor,” said Nurez Madhany, director of quality at True Health, an FQHC with seven locations in Central Florida. “It’s all of the factors, or at least the majority of the factors. And almost all of those patients are, by default, lower socioeconomic status.” The more barriers patients face to accessing care, the harder it is to get them in the door for an annual wellness visit, especially when they’re not necessarily feeling sick.
True Health CEO Janelle Dunn agreed. “As an FQHC, we face different barriers trying to connect with our patients at community health centers than private practices do,” explained Dunn. “Oftentimes, our patients don’t keep the same phone number from month to month. It is very difficult to remind them of their appointments when their phone number and/or address is transient.”
Connecting patients with community-based resources
The solutions to these challenges aren’t always clear. But meeting patients’ social needs is an essential part of care management for high-risk patients.
Given the lack of national safety net, care management staff need to be able to access community-based resources that help address needs like food, housing, and transportation. Because this model relies on the care manager’s ability to build personal connections with patients and know the community’s resources, it’s helpful for staff to be both local and embedded in the organization.
As part of the chronic care management program at Jersey Coast Family Medicine, office manager Christie Ciszewski says that the team proactively reaches out to high-risk patients to check in and find out what social supports they need. “We do a phone call that’s very social-based,” said Ciszewski. “Have you been able to get your meds, especially during COVID? Do you have someone getting groceries? Oh, now you can’t drive? Let’s set you up with local transportation.”
Many practitioners shared that patients often can’t make progress toward their health goals until their social needs are met. For example, a diabetes patient who’s also struggling with food and housing insecurity won’t be able to focus on improving their diet, exercise habits, and medication adherence without additional food assistance.
Embedding social programs within the organization
There’s variation in organizations’ ability to address patients’ needs depending on factors like financial structure and system affiliation, but many organizations also offer their own resources that are easy for patients to access. Organizations we spoke to mentioned embedded programs like substance abuse counseling, diabetes education programs, and tai chi classes, to name just a few.
True Health’s goal is to provide wraparound services for its patients, Dunn says. Those services include everything from employing Certified Application Counselors who help patients apply for Medicaid and food stamps to offering free bus passes to help patients get to their appointment.
“For patients who we know have issues with transportation, we can mail a bus pass to their house so they have it ready in advance of their visit,” said Deana Montella, chief nursing officer at True Health. “Luckily all our health centers are on a bus line, so that’s really important for those patients who have a transportation barrier.”
Above all, Ciszewski says that the one thing her practice’s healthiest high-risk patients have in common is support. “It’s someone who’s keeping an eye on them, who can run to the pharmacy, who can run them to the office, who’s helping coordinate everything,” said Ciszewski. “It’s knowing that no, their father can’t come home from rehab yet because he’s a fall risk.” Family members often play this role, but in their absence, healthcare organizations can step in to support their patient as a whole person, in support of their whole health.