Adopt these best practices to improve same-day resolution rate
For many medical practices, the end of business hours doesn’t actually mean the end of the workday. Instead, clinicians log in after hours — often from home, often in pajamas — to finish patient documentation. This “pajama time” has become an unwelcome norm across the industry.
But it doesn’t have to be that way.
Improving chart-closure rates, especially achieving same-day patient encounter completion, can help streamline your operations, reduce burnout, and help your practice get reimbursed more quickly. The key lies in a combination of optimized workflows, harnessing the power of an AI-native EHR and generative AI tools, and a culture that supports efficiency without compromising quality of care.
These aren’t just hypothetical ideas. These insights come from analyzing data from the athenahealth® network of more than 160,000 physicians and clinicians.1 Which of these best practices do you currently follow — and which ones could you add for even greater efficiency?
1. Optimize clinician workflows
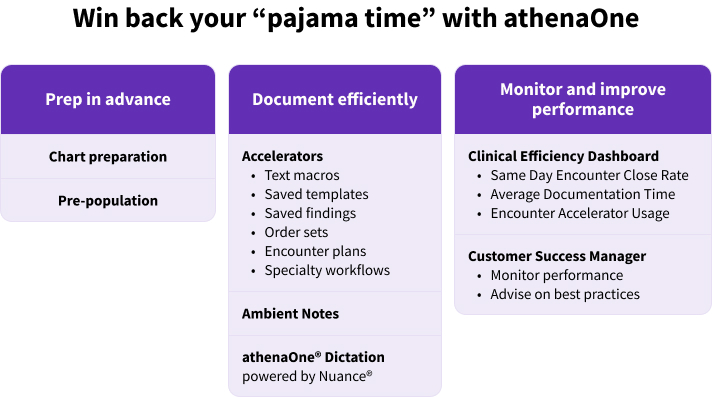
Optimizing clinician workflows involves ensuring that everyone, from physicians to nurses to medical assistants, is operating from the same playbook. For instance, a practice can set documentation time goals, encouraging clinicians to finalize all notes within a few hours of a patient encounter. As benchmarks become available, practices can use those to set realistic and achievable goals for their clinicians.
athenaOne® customers can also assign pre-visit and post-visit tasks, making it clear what each person’s responsibilities are. By delegating pre-visit intake documentation to nurses or medical assistants and having post-visit summaries and coding suggestions ready for clinicians to use, a practice can free up the clinician to focus on the components only he or she is qualified to complete.
2. Use automation and clinical AI tools in the EHR
Closing patient encounters faster starts with improving efficiency throughout the encounter itself. Automation and clinical AI tools can play a prominent role here — and physicians are increasingly optimistic about their potential to save time and effort. athenahealth’s 2025 Physician Sentiment Survey found that 68% of physicians who use AI said they’re using it more frequently to generate clinical documentation.2
athenaOne will soon boast a native AI intelligence layer built on a cloud native, single instance infrastructure. That allows for the deployment of updates to patient data sets without complex implementations or migrations. The AI-native athenaOne will give clinicians an experience where the EHR is an intelligent, adaptive partner that can help enhance decision-making and care coordination while also helping reduce administrative burden.
Generative AI tools in the EHR, such as Ambient Notes, automatically generate encounter notes based on the conversation between the clinician and the patient. Ambient Notes filters out small talk and creates the patient note for the clinician to review and approve, then proactively uploads it to the patient chart. This allows clinicians to place the emphasis on the patient during encounters while also reducing documentation time. Indeed, 3 out of 5 providers in the athenaOne network close more encounters within one day of a visit, with an average improvement of 28%.3
Soon, AI-native athenaOne will boast clinical AI tools that can help providers feel more prepared for patient encounters. Forthcoming features such as Chart Assistant and Intelligent Summaries will leverage generative AI to search across all available clinical data to help answer provider questions or generate summaries relevant to patient documents, charts, and clinical events to give providers key insights ahead of encounters. Plus, clinicians can converse with our AI assistant, Sage, or ask the assistant to help pull things like recent blood work or encounter data.
Other automative tools can also help improve same-day closures. To expedite encounter notes for routine check-ups, chronic care management, and other common situations, clinicians can leverage documentation accelerators such as templates and text macros. These EHR tools eliminate repetitive work with ease, allowing the clinician to document a typical visit, add specific details unique to the patient, and avoid having to type the same forms and phrases over and over again.
For medication reconciliation, clinicians can use a tool such as ChartSync in the athenaOne EHR. ChartSync reduces the time spent on manually entering and reconciling medication histories from other care settings. The clinician can easily view consolidated, deduplicated medication information without leaving the clinical workflow, and add it to the patient chart through automation or a click of the mouse. New ChartSync capabilities will leverage AI to read Health Information Exchange (HIE) documents, such as hospital discharge summaries, in addition to providing patient health changes since the last visit for provider review.
With ChartSync, providers can also be sure that they are getting more usable patient data. The native AI in the EHR constantly deploys updates to external clinical data which can be added to the patient chart, helping to reduce clicks and expedite same-day chart closures.
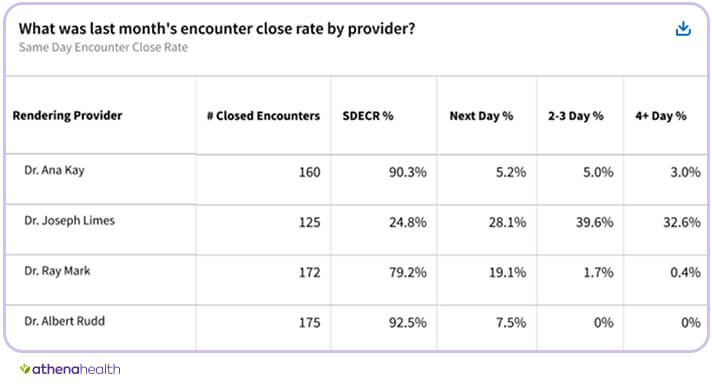
athenaOne’s Customer Success Managers meet with customers throughout the year, sharing Same Day Encounter Close Rates and other metrics, along with best practices to improve them.
3. Improve clinician training and engagement
One valuable thing a practice can do to improve its chart closure rates is help clinicians understand why it’s important and how they can improve their scores. Consider providing performance feedback during regularly scheduled meetings with the clinician. athenaOne’s Customer Success Managers meet with customers throughout the year, sharing Same Day Encounter Close Rates and other metrics, along with best practices to improve them.
Practices should also make the most of clinical dashboards, such as athenaOne’s Clinical Efficiency Dashboard, to compare performance across clinicians and specialties. Doing so can help identify those outliers who may need additional training or adjustments to their workflow.
Optimize chart completion time in 4 steps
Want to see your clinical team’s Same Day Encounter Close Rates rise? Implement these best practices today.
1. Monitor chart completion times regularly. The Clinical Efficiency Dashboard built into athenaOne can help identify outliers and areas for improvement.
2. Encourage clinicians to use documentation accelerators. In athenaOne, clinicians use macros, templates, native AI in the EHR and, and additional generative AI tools to document more efficiently and improve their same day resolution rates.
3. Train clinicians on best practices for encounter efficiency.
4. Use benchmarking data to set practice-wide efficiency goals and improve operational workflows.
Practice with peak efficiency — and put an end to pajama time
If you’re ready to improve your chart closure rates, get in touch. From network-enabled insights to one-on-one consultations with our expert Customer Success Managers, athenaOne can help you find the efficiency you seek. Set up a call today.
More electronic health record resources
Continue exploring
1. Based on athenahealth data as of Dec. 2024; M010
2. 2025 Physician Sentiment Survey of 1,001 physicians nationwide, commissioned by athenahealth and fielded by Harris Poll, Jan. 2025
3. Based on athenahealth data as of May 2025 for providers who onboarded on Ambient Notes from Feb-May 2025, with three months of consistent Ambient Notes usage and at least 10 encounters per month; M264









