Article
'Dear healthcare leaders: Your workforce is changing'
By Diane Shannon, M.D. | March 2, 2018

Dear healthcare leaders, board members, and interested others:
You may have noticed a recent trend in your human capital. If you haven't, here's the upshot: Your physician workforce is changing.
And to guide your organization, you'll need to understand those changes — and shift your priorities accordingly. As a physician and author dedicated to helping my clinician colleagues thrive, I'm here to help.
Here's how your workforce is evolving:
More women are becoming physicians. In 2017, the number of women enrolling in U.S. medical schools exceeded the number of men for the first time, according to data from the Association of American Medical Colleges. Similarly, a 2017 survey of 18,000 physicians in 3,500 practices on the athenahealth network found that 60 percent of respondents under the age of 35 were female.
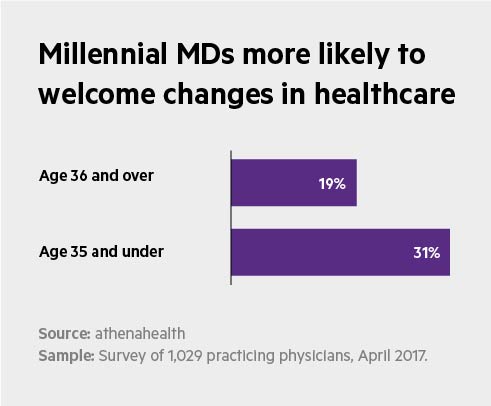
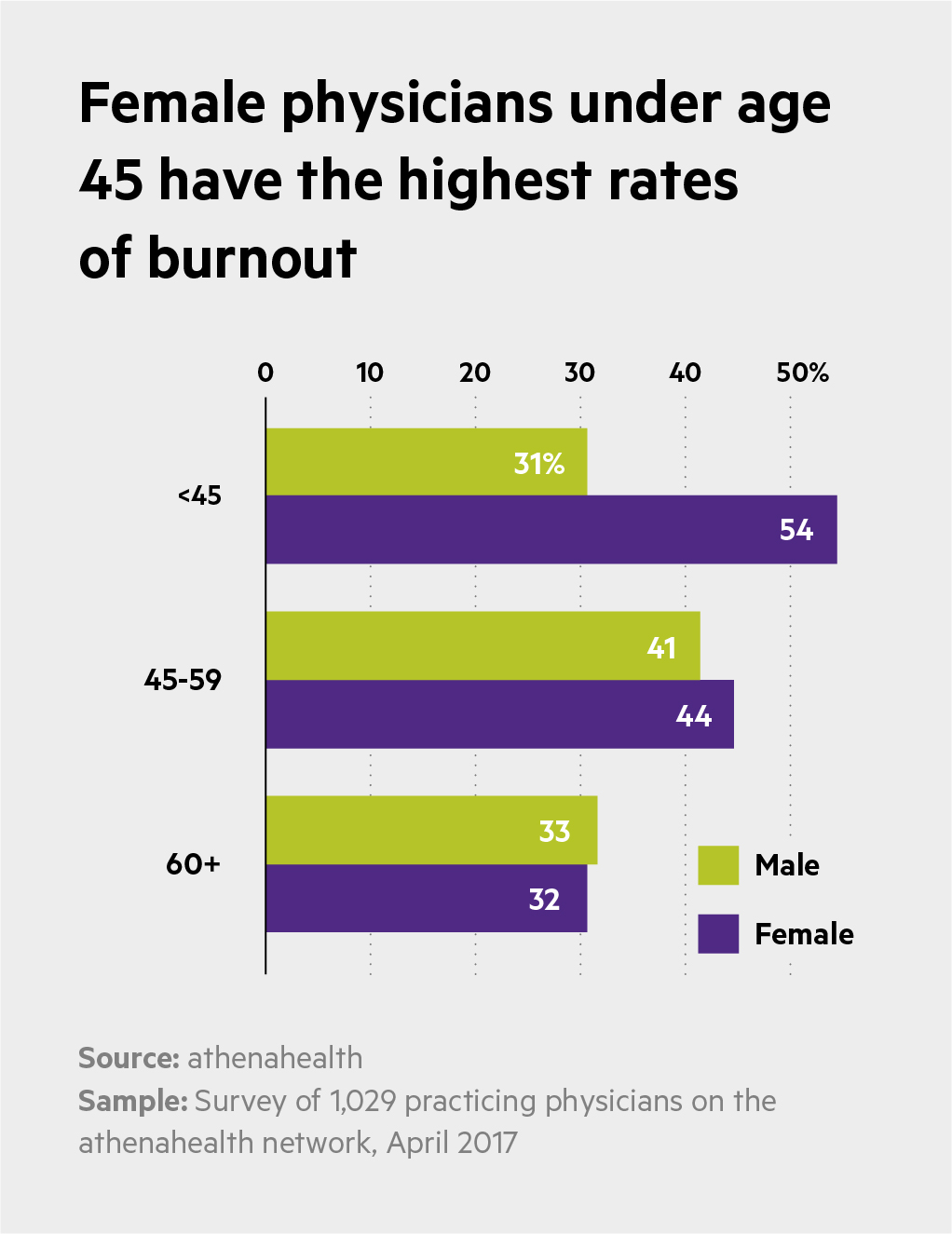
Millennials are reshaping work expectations. The millennials (ages 21 to 37) now outnumber baby boomers. Research by athenahealth show physicians in this generation are more likely to welcome changes to healthcare than older physicians. At the same time, they tend to be more concerned about adverse working conditions and stressors that affect work-life balance. And data show they're right to be cautious. According to athenahealth data, female physicians are more likely than men to experience symptoms of burnout, with women younger than 45 at the highest risk.
Younger physicians prefer to be employed. The lure of owning one's own practice is receding, as younger physicians distance themselves from the overhead and administrative tasks associated with private practice. According to a 2017 Medscape survey, only 21 percent of medical residents anticipate owning a stake in a practice, compared with 26 percent in 2015. Overall, more than half of physicians today are employed.
Women are overdue in the corner office. Although senior leadership in healthcare is still primarily male, the corps of highly trained female leaders is growing. And research indicates that breaking down the gender barrier is good for business. A survey of more than 21,000 companies across the world found that those with both women and men in positions of leadership were more profitable than comparable firms led solely by men. The researchers calculated that moving from no women in leadership to 30 percent female leaders translated into a 15 percent increase in profitability.
Nurturing the new cohort
If leaders don't prioritize the values and needs of this new physician pool, intentionally creating optimal working conditions and career support, they risk creating a workforce prone to burnout and attrition.
The newer cohort of physicians are increasingly vocal about what they expect for themselves and their patients. These doctors want more time with patients to create the healing interactions that drew them to the profession in the first place. They want to spend evenings with family and friends, not their electronic health record.
And they want agency and latitude — or what athenahealth researchers call 'physician capability': Having the tools and resources they need to give the kind of care to their patients that drew them to the profession in the first place.
Five steps to take now
Here's a game plan to attract and retain this new breed of physicians:
Conduct a self-evaluation: A 2015 study from the Mayo Clinic identifies 12 key traits of leaders, from empowering physicians to do their job to keeping them informed about changes, have been shown to increase engagement and reduce burnout. How many describe your approach to leadership?
Ensure physicians' voices are heard: Vancouver Clinic, a 250-member multi-specialty group in Oregon, worked with its physicians to develop a vision statement. Physician engagement improved, as did their relationship with administrators. Now the physicians are involved in every large decision made in the organization.
Support physician wellbeing, both culturally and operationally: Does your RVU-based compensation model incentivize skipping vacations? Find ways to encourage physicians to take time off to recharge. Enable flexible scheduling wherever possible to reduce stress among physicians with families and other responsibilities beyond the clinic.
Remove workplace barriers to time with patients: New models of team-based care enable streamlined workflows, like pre-visit planning, that remove non-clinical tasks from physicians' days.
Address glass-curtain issues: Does every physician have path to growth in your organization? Mentorship programs, recruiting leaders from a wider pool of candidates, and flexible work arrangements can address demographic imbalances in leadership.
Acknowledging and adapting to changes in the face of the physician workforce is critical to the viability of healthcare organization — and to ensuring that patients get the care they need.
Diane Shannon, M.D., is a writer based in Boston and the coauthor of Preventing Physician Burnout: Curing the Chaos and Returning Joy to the Practice of Medicine.






