Article
Where telehealth is taking off: Rural America
By Jenni Gritters | April 6, 2017

Months later, the patient was in remission. At the time of her diagnosis, her primary care provider hadn't yet heard about the UC Davis therapy. It's likely that without the telehealth consult, she would have died.
Her experience underscores the potential — and the need — for telehealth in rural communities.
“In rural states, many people have trouble accessing specialty care, and healthcare wait times are long," says Veenu Aulakh, executive director of the Center for Care Innovations. “Telehealth is taking off out of pure need and no other option."
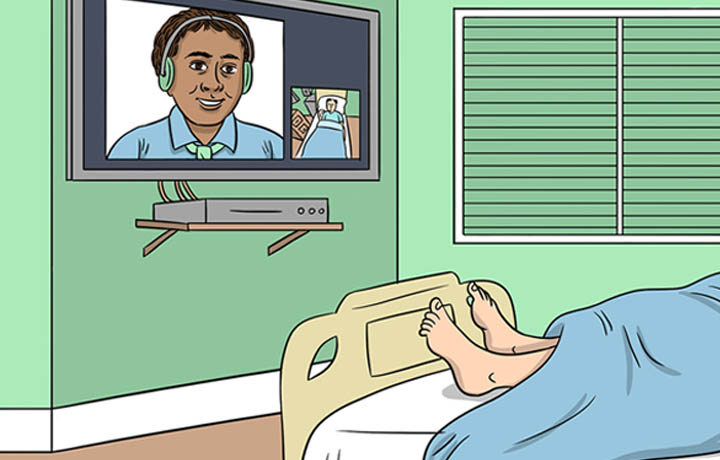
The term “telehealth" covers many technology-based medical practices, including image-based consulting, e-consults, remote patient monitoring, and mobile health tools. Remote consults have been happening for decades, with a reported 16.6 million online care consultations occurring in the U.S. in 2015.
But as Aulakh explains, telehealth has taken off in recent years out of necessity, especially in rural areas where hospitals are going out of business in alarming numbers. The technology can be especially useful, experts say, in regions where patients suffer from chronic conditions, and need tools to help them contact clinicians and engage in their own care.
“If you talk to people, the biggest complaint about healthcare is often access to their doctors. Telehealth connects those pieces of the puzzle," says Glen McCracken, M.D., founder of eVisit, a telehealth software company that is a member of athenahealth's More Disruption Please program.
The photo that saved an ear
Traditionally, medical specialists tend to cluster around academic medical institutions in large cities, which leaves many rural populations without easy access to quality healthcare or specialists. But as telehealth options become more common, high-quality care is a videoconference or phone call away for most rural patients. That's a game changer.
“Telehealth brings big-city medicine and the latest knowledge and tech into rural communities, where primary care providers often don't have time to learn about the latest technology and medicine," says Kathy Chorba, executive director of the California Telehealth Network.
Chorba recalls a patient from Weaverville, California, who came into the emergency room with a rash on her ear, for which the doctor prescribed an antibiotic. The rash worsened, and after several more visits, the physician was at a loss. He told the patient he might need to remove her ear.
But before he could move forward, a nurse sent a photo of the ear and the patient's records to a well-known dermatologist at the University of California, Irvine. Within hours, the dermatologist responded via email: “Patient is allergic to meds."
Within a week, the patient was off the medication and healed — and she got to keep her ear.
The story illustrates another telehealth benefit for patients and providers in rural areas: the opportunity to learn from one another. In another part of California, a rural physician referred more than 17 HIV patients per month to a specialist at an urban academic medical center. The monthly referral number soon dropped to 15, then 10, then 5.
The reason? As the physician attended tele-consults with her patients, she learned from the specialist, which allowed her to practice at the top of her license and bring better care to her community.
“For providers who work in the space, it can be frustrating, knowing that patients desperately need better access to care," Aulakh says. “From a provider side, telehealth makes sense: You provide their patients with the access they need, and you learn."
Challenges to connection
Experts say the clearest wins in telehealth so far have come in rural areas, in the form of image-based consulting work and increased access — and less travel — for postoperative patients.
Still, much work remains to be done if telehealth is to reach its potential for empowering rural communities. Among patients on the athenahealth network in 2016, enrollment in physician portals was nearly twice as high for urban patients as for their rural counterparts. Existing telehealth platforms are generally impressive, but innovators need to turn their attention to contextual barriers: Physician acceptance, reimbursement processes, and access to high-quality, secure internet connections.
Telehealth currently exists primarily in rural clinics, where the work is generally reimbursable by insurance companies. But experts predict that in the future, telehealth services could extend to the home, which makes the reimbursement equation more complicated.
Additionally, access to secure, fast broadband internet can restrict the level of long-distance care physicians can provide. California recently implemented HIPAA-compliant broadband for medical facilities, which makes clinic-to-clinic telehealth consults much easier.
But most rural communities lack access to high-speed wireless. If a patient wishes to engage in a video tele-consult from home, finding a reliable, secure internet connection still presents a major problem.
Despite the barriers, though, telehealth is becoming increasingly essential for Americans living in rural communities — and is empowering both rural and urban patients to seek better care.
“In three to five years, I think every practice in the U.S. will be using telemedicine in some way," McCracken says.
Aulakh agrees. “Getting people to change past behaviors is the challenging part," she says. “But we're doing everything else remotely in our lives. It feels like we have to move this way."
Jenni Gritters is a journalist based in Boston.
Image credit: Getty Images