Article
What does it take to achieve quality?
By Josh Gray |

We used our unique data set — which offers a near-real-time view into the actions of health systems and medical groups — to find the best performers among our nationwide network of 88,000 providers. We interviewed them to isolate the factors that account for their success. And by analyzing their practices, we began to develop a theory of operational excellence.
Now, we've expanded our research to examine an issue that is top-of-mind for organizations eyeing the shift to value-based care: The quality measures that drive both reimbursement and patients' health.
How to define and measure “quality" remains a hot-button topic in healthcare, especially as provider organizations grapple with different sets of quality measures across multiple payer contracts.
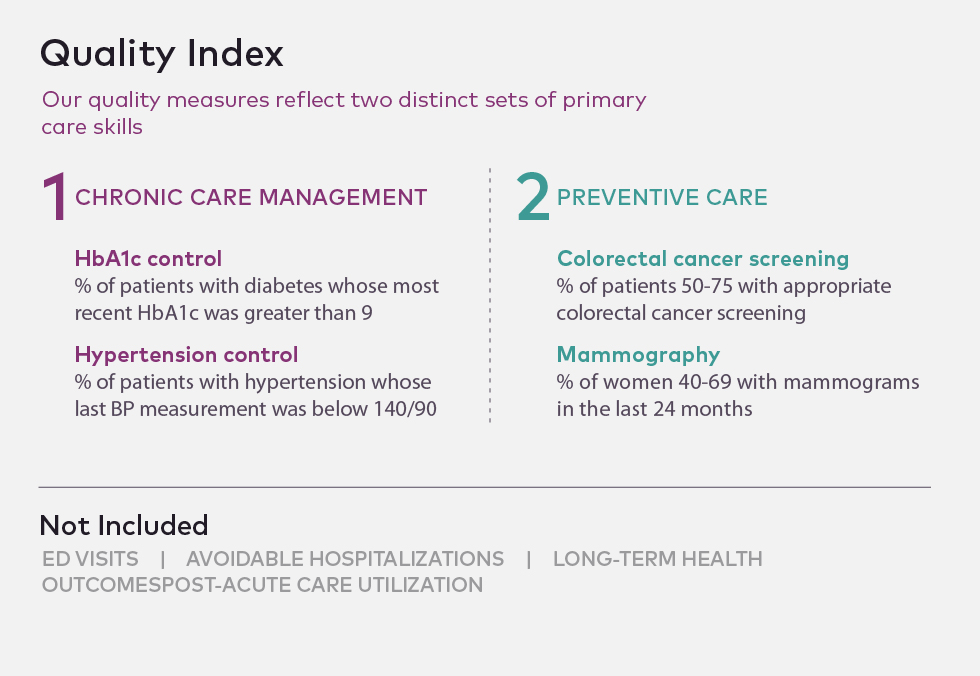
None of these measures are perfect, and some of these procedures might be delivered by specialists. Nevertheless, a primary care doctor should have a record of screening procedures, and each of these measures is often included in payers' pay-for-performance calculations. Primary care providers should be in charge of coordinating patients' overall health needs, and so it is essential that they be aware of and accountable for performance on these measures.
While these metrics don't reflect important inpatient data such as avoidable hospitalizations and emergency department use, or more comprehensive measures such as total healthcare spend, they are core to many pay-for-performance contracts and reflect chronic disease management as well as critical screening procedures.
These four measures, combined into a quality index2, provide a defensible proxy for an organization's success in achieving quality outcomes.
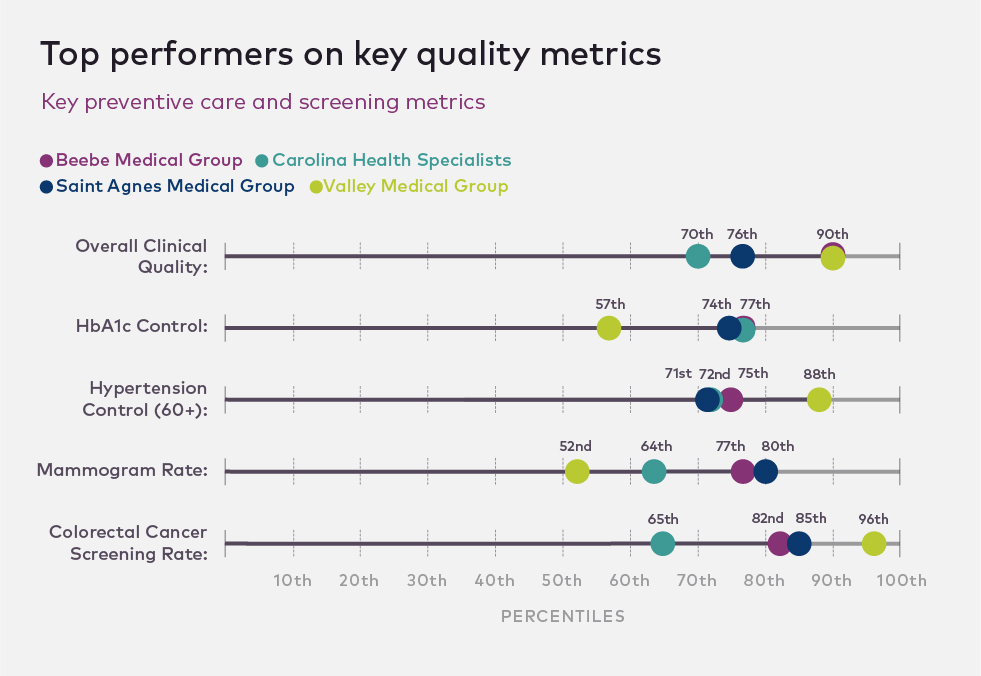
Using this index, we've identified 16 top performers and interviewed them extensively. High performers were designated as organizations that fell within the top 30 percent of the network for the quality index.
Key performance insights
First, for both ends of the performance spectrum, financial results and clinical quality align. The median physician group in the top quintile on financial performance is in the 65th percentile on quality metrics. The median physician group in the bottom quintile on financial performance is in the 33rd percentile on quality metrics. This makes sense; top performers have missions, workflows, and tactics that keep them focused on results in multiple domains.
Second, our top performers' best practices fall into the same three dimensions of organizational capability that our research has identified as core to financial performance: physician and staff capability, patient capability, and leadership.
High-performing organizations design smart workflows for staff to ensure the comprehensive capture and reporting of quality measures. They seize every opportunity to close care gaps while engaging patients to be more active and capable participants in their own care. Their leaders have a vision — and a strategy for hiring and communicating — that helps position them for sustainable growth and the transition to population health.
The third insight is that high-performing organizations tend to share a set of organizational and cultural attributes that they regard as foundational to their success. Most, for example, have a strong physician voice within leadership; deploy incentives strategically by engaging physicians and staff on a variety of goals, not simply rewarding productivity; and embrace an ethos of radical data transparency, sharing unblinded performance data and encouraging discussion of best (and worst) practices.
Physician and staff capability
Our high performers operate with clearly defined staff protocols, which follow a simple precept: Physicians should lead quality improvement efforts — redesigning care delivery to improve outcomes at lower cost — but they should not be responsible for quality reporting.
Too often in practices, the burden of capturing and reporting quality measures falls on the shoulders of the physician, interfering with the physician-patient encounter. We found that the most successful organizations delegated this reporting to clinical staff, putting in place protocols that ensure providers ask the right questions and document the answers properly.
As a practice administrator at Carolina Health Specialists, a 50-provider multi-specialty group based out of Myrtle Beach, South Carolina, told us: “The clinical staff handles quality management on behalf of the physician. So, it doesn't really impact the physicians. Some of them don't even recognize that they're fulfilling these requirements because the clinical teams are taking it on for them."
Pre-visit planning is essential to ensure patients receive needed care. In some high-performing practices, cross-functional teams that include nurses and medical assistants meet before patient encounters to identify gaps in the patient's medical history (such as vaccinations, screenings, and unfilled prescriptions).
“The idea is to 'stretch the visit' so it doesn't just happen in those 15 minutes. It starts a week before, when we're reviewing the record. It's a few days before, when we get their lab results, and it happens after the visit when the patient gets a care summary," explains Joel Feinman, Ph.D., president of Valley Medical Group, a 100-provider independent physician group in western Massachusetts whose strategies have established them in the top 10 percent of our quality performance measures.
High-performing organizations also take deliberate steps to make sure patients do their part in managing their health — which includes getting routine care and screenings. They don't assume that all patients will come in for physicals or annual wellness visits, so they use sick visits as opportunities to check in and close gaps in clinical care.
Mindful of limited resources, high-performing practices focus their efforts where they are likely to have the greatest impact, calibrating effort against patient risk levels. As part of their pre-visit planning process, some practices deploy nurses and medical assistants to review charts before appointments to identify a patient's care gaps: Why hasn't this patient re-filled a prescription that has run? Has he had high blood pressure in the past?
Front office staff schedule frequency of follow-ups based on risk levels and care managers reach out to patients at the highest risk. Physicians follow evidence-based guidelines for prescriptions, testing, and visit frequency, especially for complex patients.
Patient capability
Sometimes, workflow changes like these are essential to capture the right quality data and make sure well-managed patients stay up-to-date with their medications and screenings.
But with some populations, particularly those that face multiple chronic conditions, it is particularly important that patients are actively engaged in their own care. Their health and clinical outcomes depend on keeping them motivated.
So, high performers pay close attention to the patient journey, and take extra steps to enable what we think of as the “job of the patient," giving them the tools and support they need to adhere to medications, fulfill prescriptions and referrals, change lifestyle habits, and the like.
High performers acknowledge the critical role of the patient in their own healthcare — and some even hold patients accountable if they fail to meet their commitments.
For instance, Beebe Medical Group, a hospital-affiliated physician group in Delaware in the top decile for quality metrics in our index, will reschedule follow-up visits if patients show up with incomplete lab work or if they haven't followed through on referrals, which occurs around 10 percent of the time. If the patient has done his job before the visit, the physician has the time and knowledge to do her job during the encounter.
Another organization conducts aggressive outreach to its patients, describing how they “walk the line between persistent and annoying — because it's right for the patients." Of course, the goal is to empower and equip patients to do their jobs, not to penalize them.
Leadership
The top performers we spoke with are at very different points on the road to taking on the risk for managing populations, largely based on payer dynamics within their regional markets. Wherever these organizations are, however, their leaders are intentionally taking a phased approach to the transition to risk-based reimbursement.
While maintaining a focus on the foundational quality metrics in our index, these groups are forging a slow but steady path, recognizing the substantial transformation and financial risk involved. Some high performers, for example, are changing their service mix by prioritizing specialties — such as behavioral health — that are important under both fee-for-service and risk-based contracts.
High-performing groups often pilot small-scale innovations before introducing more broad-based and disruptive changes. Saint Agnes Medical Foundation in Fresno, California is one example. In the top 15 percent for most quality metrics on our index, they have the greatest opportunity to improve their management of diabetic patients, where they are in the 73rd percentile.
The medical leadership at Saint Agnes is investing in a redesigned diabetes management infrastructure, which they expect will help them achieve cost targets under risk. They are starting modestly, piloting a high-touch initiative in one of their practices that will have a diabetes nurse educator keep close tabs on a small, high-risk patient panel.
In short, they are undertaking a classic “lean innovation" approach, working out the kinks in pilot, finding out what works and what doesn't — so that when the time comes to move to full-risk contracts, they will be prepared to roll out a proven model for managing their sickest patients. In the meantime, they are not breaking the bank investing in infrastructure their contracts don't reimburse, or taking focus away from their existing, reporting-based quality efforts.
What's next?
A proliferation of quality initiatives has left many providers unsure of where to focus their attention to achieve meaningful improvements. Federal payers have sought to define and incentivize providers to achieve quality through PQRS, MIPS, and other programs. Many provider organizations focus on quality performance as a critical foundation for making the shift to population health and value-based reimbursement.
Our network data gives us the ability to find the organizations that are already succeeding. In coming weeks and months, we'll be shedding light on their innovations and successes, sharing their stories and tactics, with the goal of helping all healthcare organizations find a path to measurable improvement.
We will continue to monitor our network to identify practices that are elevating quality, and probe the connections between operations and outcomes — examining, for instance, the links between provider and patient engagement levels and clinical performance. We expect many more insights to come.
Josh Gray is vice president of research at athenahealth.





