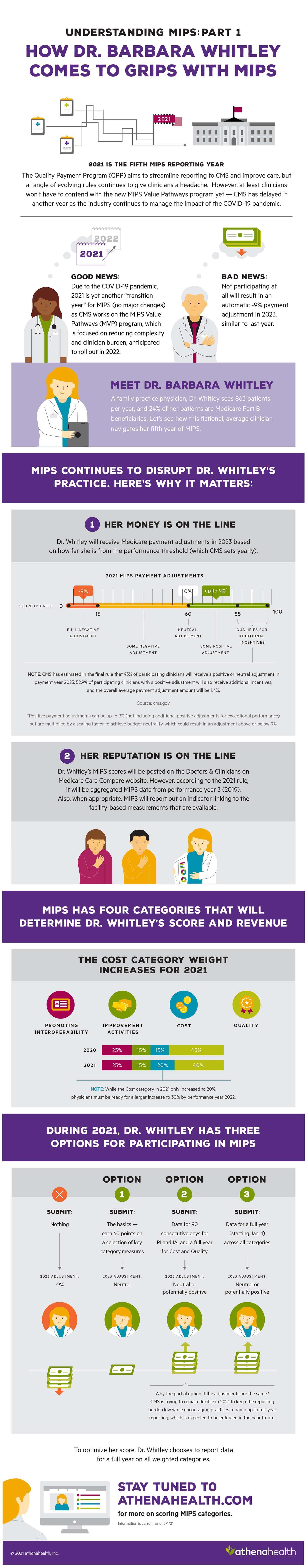
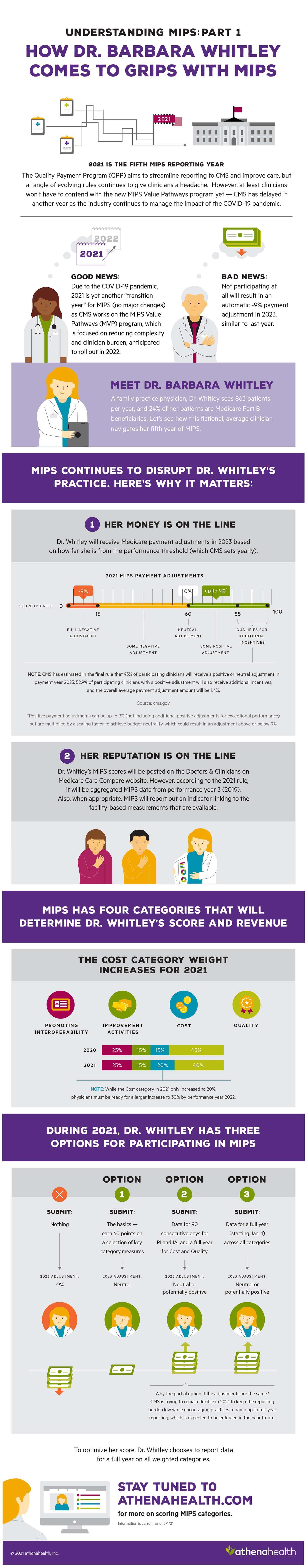
Infographic
Demystifying MIPS, an overview
Discover how athenahealth helps organizations succeed with quality programs.
close
Want to hear more?
Get insights from athenahealth’s open and connected ecosystem delivered right to your inbox.
Sign UpInfographic
Discover how athenahealth helps organizations succeed with quality programs.