Article
Expert Forum: Decision fatigue and antibiotics
By Chelsea Rice | June 1, 2016

It's known as decision fatigue, a sociological phenomenon that has been studied across all aspects of daily life — from dieting to shopping to the judicial system. And health care isn't immune. Providers are packing more appointments into every day and making dozens of decisions within a single appointment — arguably more than ever, thanks to the demands of quality programs.
So Hannah Neprash, a PhD candidate in health policy at Harvard University, studied athenahealth network data to explore how decision fatigue might affect the clinical judgment of providers over the course of the day — through an analysis of antibiotic prescribing patterns.
"Medicine seemed like such a ripe area [to examine decision fatigue], because physicians are a great example of folks who make both a lot of decisions in one day and also really important decisions," Neprash says. She focused on antibiotic prescriptions because doctors are frequently confronted with the choice — and pressure — to prescribe the drugs, and because of concerns about the risk of antibiotic-resistant "superbugs."
In outpatient care, 13 percent of all visits result in an antibiotic prescriptions, according to a recent Pew Charitable Trust analysis of data from the Centers for Disease Control and Prevention. Fully 44 percent of those visits are related to acute respiratory conditions that should have been resolved without antibiotics. For at least half of these diagnoses, antibiotics are ineffective. But that doesn't stop patients from asking for them.
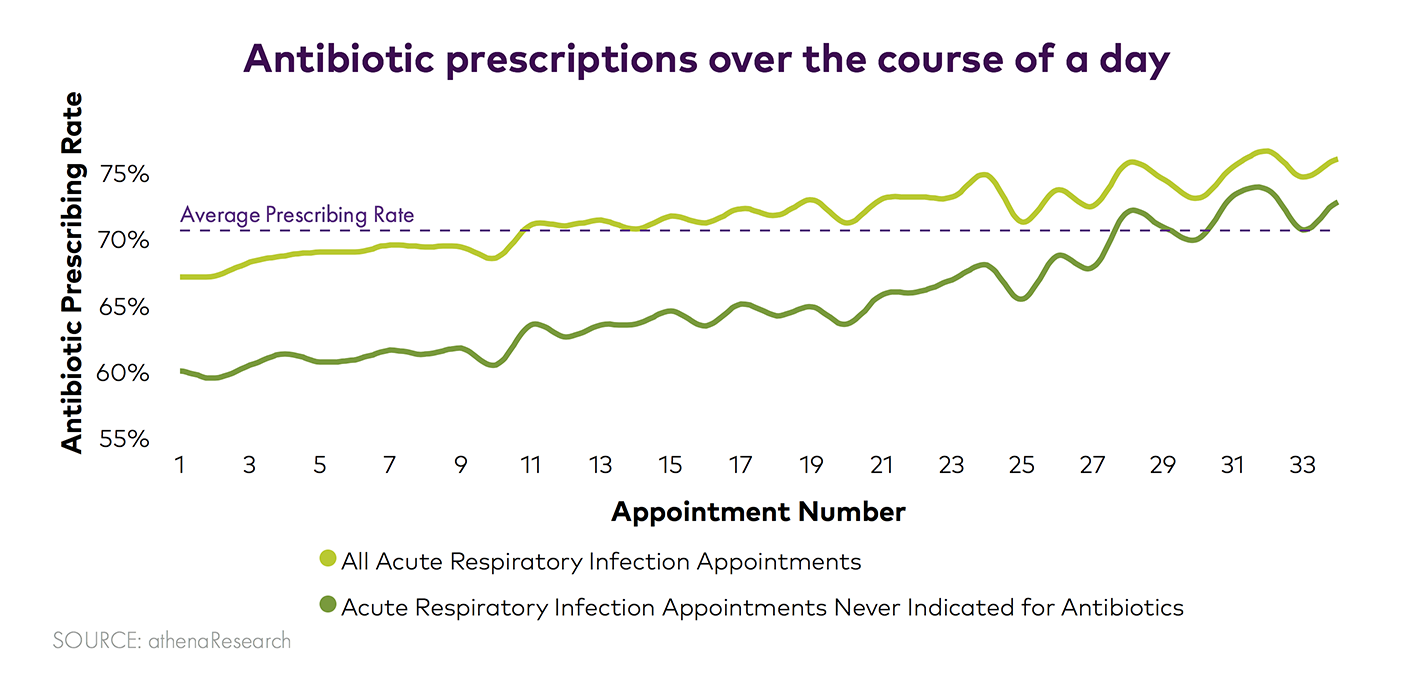
Neprash reviewed more than 175,000 interactions on the athenahealth network between primary care providers and non-elderly adult patients who displayed symptoms of acute respiratory infection. She found that over the course of the day, the rate of antibiotic prescriptions rose significantly.
Doctors were 13 percent more likely to prescribe an antibiotic in the 13th appointment of a day and 19 percent more likely by the 24th appointment. The data mirrors similar 2014 findings published in JAMA Internal Medicine and recently summarized in the New York Times.
So, are the cards stacked against providers? athenaInsight asked some experts for their thoughts. Their condensed answers are here:
Ann Thomas MD, medical director for Oregon Health Authority's Alliance Working for Antibiotic Resistance Education (AWARE) program
It's not so much that doctors get tired and make bad decisions; it's that there's this interplay of negotiating with the patient. And what happens is that all patients come in wanting antibiotics. At least that's how most clinicians will feel: They know that they shouldn't be giving antibiotics, but patients want them.
When you're fresh, and it's the beginning of the day, you are more inclined to have this full conversation that usually goes something like: “Well, I think that what you have is a viral infection. And I really would not want to give you antibiotics, because I think it's more likely to cause side effects of diarrhea, or some rare anaphylactic reaction in you, than it is to help your infection — along with the fact that it promotes antibiotic resistance, and you could end up with an infection that might not be treatable."
Anecdotally, if you just talk to doctors, most of them will give the impression that they can talk patients out of antibiotics, but it takes more time. So the fatigue is just that wearing down and not being willing to [talk the patients out of it]. When it's at the end of the day and you're behind and you're tired, it's like, “Okay, I'm just going to give it to them. That's what they want, and I'm going to get them on their way."
It's not decision fatigue — it's 'talking with patients all day fatigue' or 'patient negotiation fatigue.' And I think most clinicians feel that if they're going to provide good care and to talk patients out of antibiotics, that they need to spend more time talking.
David R. Andes MD, professor of infectious disease, University of Wisconsin School of Medicine and Public Health
It's probably just human nature. Strategies to get around this problem are obviously needed but it's doubtful that seeing fewer patients will be a viable option. So improving workflows — particularly workflows around patient education — may be the most helpful.
It's important to consider what other factors could come into play later in the day: Does this happen in morning or just afternoon clinics? Patients may be worn thin by end of the day as well, so it may be that patients themselves are more demanding. This shouldn't all be on the clinician.
You should consider, too, whether the other clinic staff are not as patient or not as good at educating. Or are they even helping to educate? We know a team approach is best for solving this. Whether front desk folks or education tools that can be marketed to patients are most effective to relieve the burden on the doctor, that remains to be seen.
When clinicians [at our hospital] have been made aware of the issues regarding prescription of the wrong antibiotics — or prescription of antibiotics when they aren't needed — we've seen quite a turnaround. A little sunshine helps in this area. When we recognize the prescription of an antibiotic that's not optimal, we address the clinician immediately.
Roy Baumeister, Francis Eppes Professor of Social Psychology at Florida State University and co-author of "Willpower: Rediscovering the Greatest Human Strength," a New York Times best-seller about self-control and decision making
It doesn't matter where you expended your willpower, whether it was resisting the doughnuts or dealing with marriage problems or work stress or whatever. Another doughnut impulse arises, and when your willpower is low, you decide to eat. Neither of those decisions was there in our evolutionary past, when the brain formed. But in general, the brain does register differences in importance, with some limitations.
All willpower comes out of the same pot. In the abstract, it's probably just as easy to prescribe one thing as another, but there is pressure from the patient to give the antibiotics. It's resisting that — including explaining — that depletes the person and changes the outcome. Simple decision fatigue does not change the outcome of the decision process unless there is some kind of inner or outer pressure to do the wrong thing.
Image credit: Education Images/Getty Images, Nicholas Page






