Article
How telemedicine can lower costs in the ICU
By Peter Barnes | July 7, 2016

Factor in additional annual costs of as much as $53,000 per bed, and it's not surprising that telemedicine is part of the care plan for only a fraction of patients who need round-the-clock monitoring.
But research from the University of California, Davis makes an economic case for expanded telemedicine — by quantifying its benefits in terms, not just of outcome, but of cost.
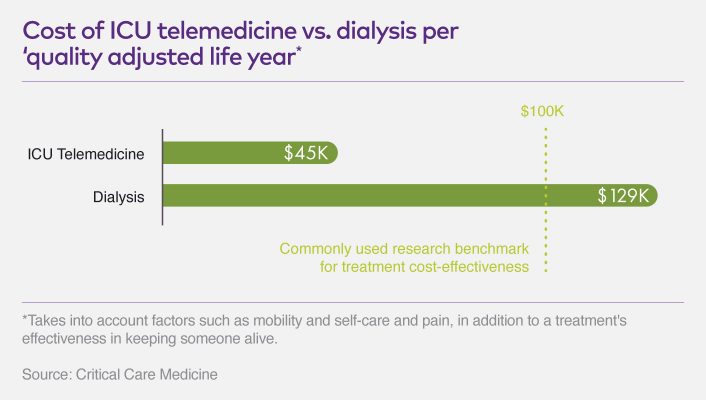
Using data from previous studies, a team led by epidemiology professor Byung-Kwang Yoo, M.D., PhD, built a mathematical model to assess the cost-effectiveness of ICU telemedicine in terms of "quality adjusted life years," a generic measure of disease burden taking into account factors such as quality of life (mobility, self-care and pain, for example), in addition to a treatment's effectiveness in keeping someone alive.
One of the team's analyses pegged the cost of ICU telemedicine at $45,320 per quality adjusted life year. That compares to roughly $129,090 for dialysis. And it falls well below the $100,000 benchmark researchers often use to define a treatment as cost-effective.
The study also offers health systems insight into variables such as per-patient operation costs, staffing and ICU mortality as they relate to whether telemedicine is likely to pencil out. According to the model, ICU telemedicine produced cost savings in 37 percent of the 1,000 scenarios it considered — and the technology was worth its expense, in quality adjusted life years, two-thirds of the time.
These results could help make the case for more consistent insurance coverage for telemedicine, while adding credibility to a tool that has drawn renewed attention from health care decision makers in recent years.
'Like a hockey stick'
Back in 2003, fewer than 1 percent of ICU beds had a remote monitoring capacity. Today, that number is closer to 13 percent, says Jonathan Linkous, CEO of the American Telemedicine Association, who estimates that more than 650,000 patients this year will spend at least part of their time in the ICU under the care of a provider located elsewhere.
And if adoption of broader telemedicine practices is any indication, he says, ICU use will continue to expand.
"The growth rate generally in telemedicine has been probably doubled in the last two years," Linkous says. "It's like a hockey stick if you look at the graph."
One reason is an increasing body of evidence showing that when patients are connected to remote providers, care improves. Among the earlier research incorporated in the modeling at UC Davis was a 2014 study analyzing anonymous medical records from 118,990 people treated at 56 ICUs around the country.
Investigators found that 10 percent of the patients treated in ICUs with telemedicine capabilities died in the hospital, compared to 11 percent in the control group. It was a statistically significant difference.
In addition, the telemedicine patients spent, on average, 20 percent less time in the ICU and 15 percent less time in the hospital. The study credited these results primarily to:
- Intensive-care specialists reviewing care plans within an hour of patient admission
- More frequent review of performance data with hospital leadership
- Increased adherence to ICU best practices
- Shorter response times for alarms
- More frequent interdisciplinary rounds, and
- More effective institutional ICU committees
Complicated cases
Much of this comes down to the number of eyes on the patient, along with access to an intensivist. The Society of Critical Care Medicine notes that this medical specialty could experience a substantial labor shortage by 2020, in the face of an aging population and improved life expectancy.
This has long been an issue in many rural areas and smaller hospitals, where telemedicine can help ensure that ICU patients receive adequate care despite staffing constraints. As Linkous notes, ICU cases can be notoriously complex, and often involve comorbidities monitored through multiple vital signs.
This has long been an issue in many rural areas and smaller hospitals, where telemedicine can help ensure that ICU patients receive adequate care despite staffing constraints. As Linkous notes, ICU cases can be notoriously complex, and often involve comorbidities monitored through multiple vital signs.
Remote monitoring isn't always needed 24/7, Linkous notes; many facilities rely on off-site physicians only at night. But the technology, he says, can fill a crucial gap.
"A lot of hospitals either don't have somebody with that training or maybe only have somebody with that training for a portion of the time," Linkous said. "That's why the studies have shown that there is a big improvement in outcomes."
Peter Barnes is a writer based in Portland, Oregon.






