Article
Pediatric PTSD as a diagnosis – and an opportunity
By Alison Pereto | July 19, 2018

According to data from more than 1.7 million pediatric patients across the athenahealth network, the number of new diagnoses for PTSD in children age 5 to 18 more than doubled from 2013 to 2017 — increasing from an average of 4 diagnoses to 8.3 per 10,000 pediatric patients.
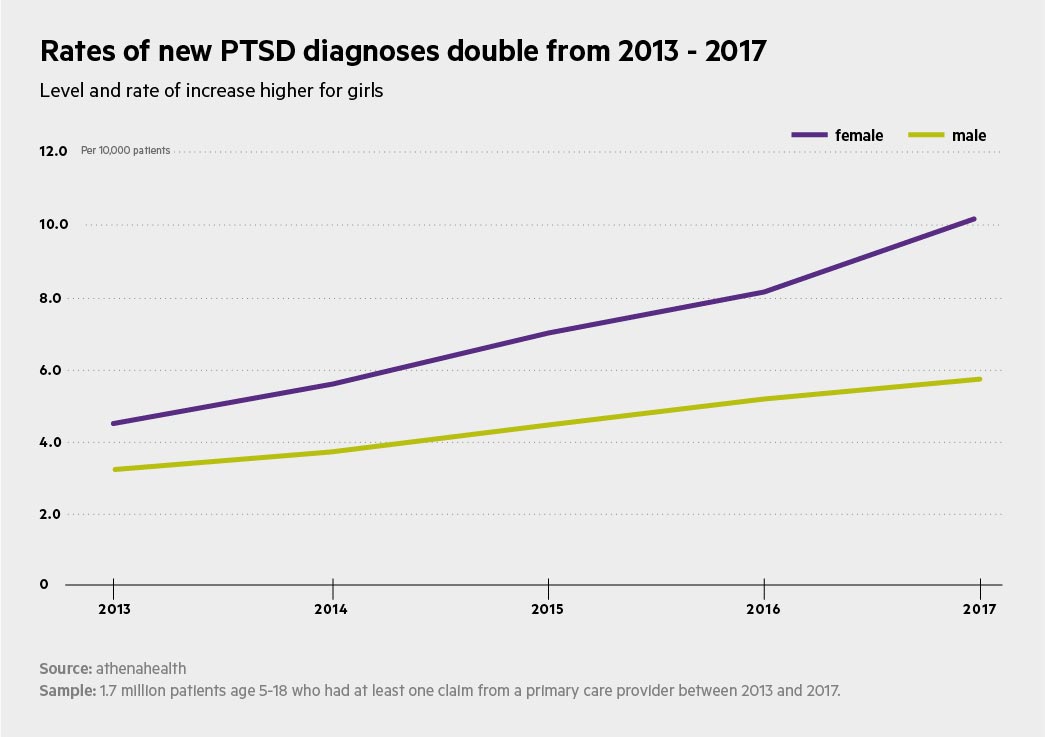
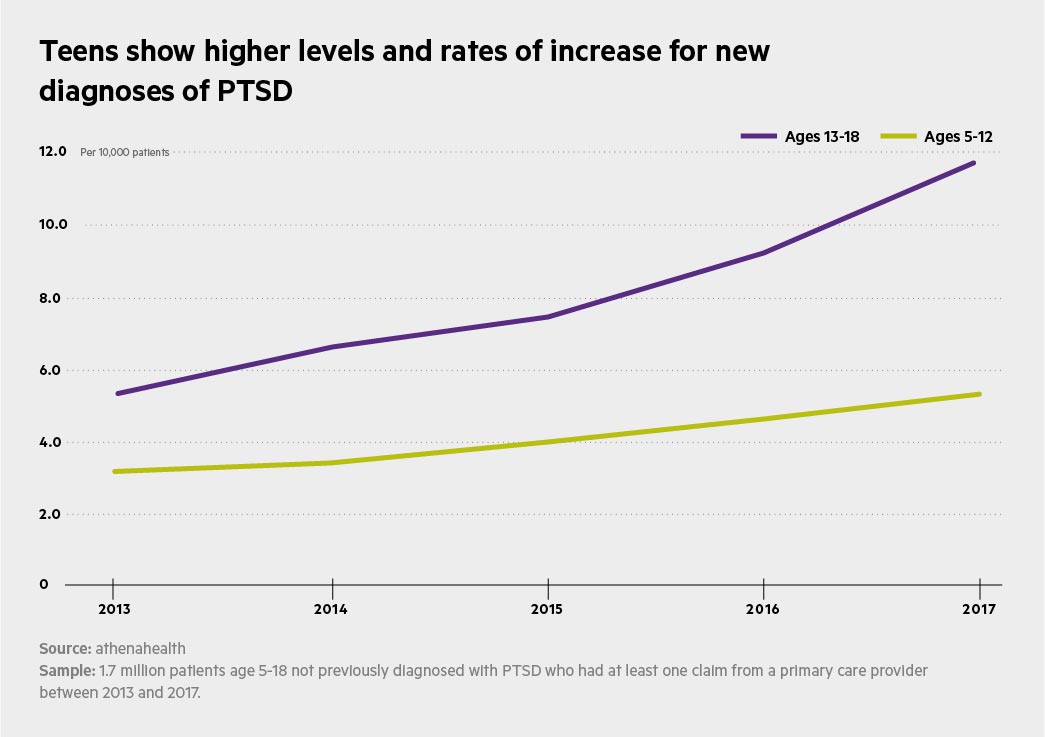
The level and rate of increase in diagnoses was higher for girls; by 2017, diagnosis rates were twice as high for girls as for boys. Similarly, the level and increase in diagnoses was higher for teens (age 13 – 18) than for children age 5 – 12. Teens saw a 126 percent increase in new diagnosis rates over the sample period, compared to a 67 percent rise for children.
"This is a dramatic change," says Claudia Gold, M.D., a behavioral pediatrician specializing in early childhood mental health and author of "The Developmental Science of Early Childhood."
“In the 20 years I've practiced pediatrics, I've never diagnosed a child with PTSD."
A diagnosis of PTSD doesn't tell a patient's full story, Gold cautions. PTSD could apply to children struggling with a single traumatic event — a car accident or assault — while others are facing ongoing trauma, anything from domestic violence to a mentally ill parent. In short, says Gold, a diagnosis of PTSD is “a dramatic oversimplification of the experience of each individual person."
As a tool in care delivery, however, a PTSD diagnosis can be useful to open doors to a range of assistance and support for children and families. And that may explain the rise in diagnoses.
It's possible, says Gold, that as more primary care providers become aware of the landmark Adverse Childhood Events (ACEs) study, they may be coding for PTSD more frequently. The ACEs study demonstrated that childhood traumas have a dose-dependent correlation with chronic illness in adulthood. When a child exhibits behaviors consistent with anxiety or ADHD, and the provider knows the child also has a high score on the ACEs scale, even a generalized PTSD diagnosis may make sense.
The athenahealth data, however, offer another clue to a possible cause for the spike: Pediatric patients on Medicaid were far more likely to receive a PTSD diagnosis than those with commercial insurance.
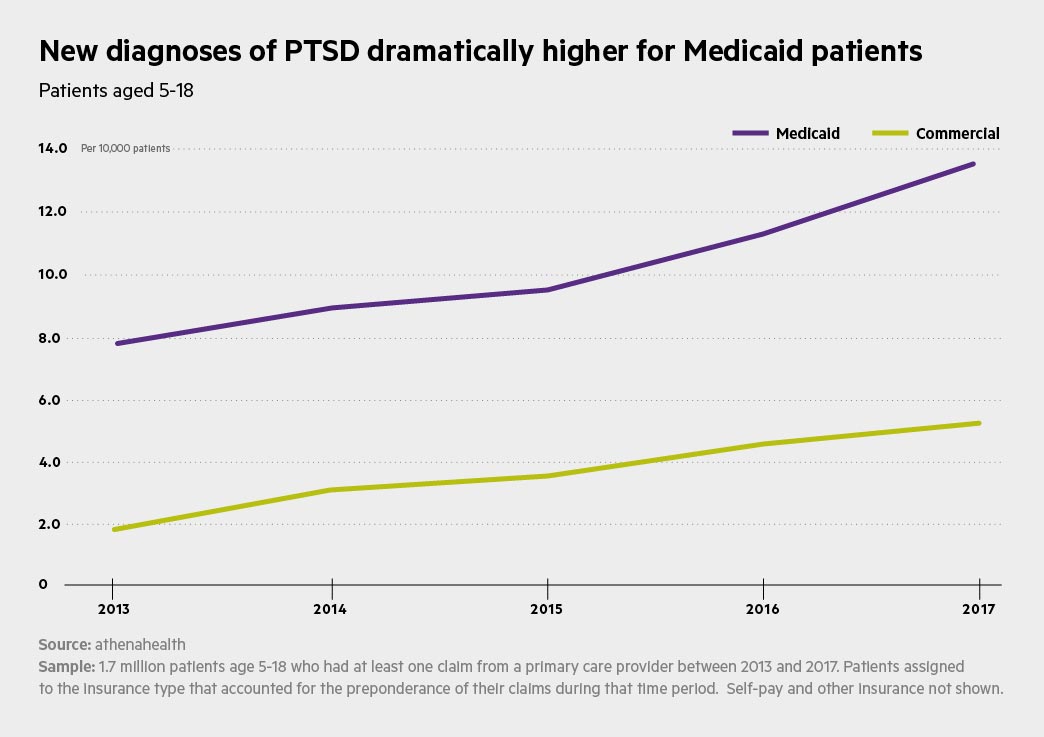
Children on Medicaid are likely to be living in poverty, and therefore at risk of food instability, violence, and other stressors. They may need a range of behavioral therapies to manage those physical, mental, and emotional stressors, but have access to few or none. Gold suggests their providers may view a PTSD diagnosis as opening a door for patients to gain access to social services.
Does that mean the diagnosis is inaccurate? Not at all, says Gold. Providers are now “paying more attention to what happens to kids – like having a substance-abusing parent, an incarcerated parent, or witnessing domestic violence – and its impact on their health.
"A primary care provider who is aware that his or her patient has experienced trauma can have a lot to offer," says Gold.
And yet even a diagnosis that leads to help from a provider and social services can have inherent risks.
“Recognizing that life experience over time has an impact on people's physical and emotional health, and then addressing that, is a really good, positive thing," says Gold. “But that thing that becomes tricky is when you call it a disorder, because then you're saying to the child, 'There's something wrong with you.'"
Instead, Gold proposes an unexpected ICD-10 code: “I would diagnose them with 'life.'" A health system that recognizes life experience as a driver of poor health could free up providers to listen to patients' stories – encounters that allow relationship building beyond checking a reimbursement code.
Listening to patients may have more impact on outcomes than coding for reimbursement, says Gold. "Imagine if every provider could say to every patient, 'You're suffering with both physical and emotional problems because you've experienced more stress in your life than your body can handle. And you need help with that.'"
Support for this research was provided by the Robert Wood Johnson Foundation. The views expressed here do not necessarily reflect the views of the Foundation.






